Healthcare providers are dedicated to delivering equitable and effective care to all patients. However, historical biases and gaps in medical research have led to disparities in how we diagnose and treat diseases across different groups. Healthcare equity is a broad concept that encompasses not only sex differences but also racial, ethnic, and age-related disparities in care offered.
These disparities are particularly pronounced in cardiovascular medicine. Women often present with different symptoms of heart disease than men, which can result in misdiagnosis or delayed treatment. According to the WHO, cardiovascular diseases (CVDs) are the leading cause of death globally, accounting for one in three female deaths each year1.
Yet, women are 50% more likely than men to receive an incorrect initial diagnosis following myocardial infarction2. These staggering statistics underscore the critical need to address sex disparities in cardiovascular care with urgency and commitment.
As we continue to celebrate Women’s Health Month, this article explores the history of sex disparities in medicine, highlighting the specific challenges in cardiovascular care for women, and the role that innovative solutions like artificial intelligence can play in bridging these gaps. Moreover, it offers actionable steps that healthcare providers can take to improve outcomes for their female patients.
Dark History of Sex Disparities in Medicine
The disparity in cardiovascular care for women has been well-documented in the medical literature, revealing a longstanding sex bias influencing research, diagnosis, and treatment protocols. Historically, medical research has predominantly focused on male subjects, often excluding women from clinical trials3. This sex bias has led to a lack of understanding of how diseases manifest differently in men and women.
The classic symptoms of Acute Coronary Syndrome (ACS), such as chest pain radiating to the left arm, are based on studies conducted predominantly on men. Women, however, often experience subtler symptoms such as fatigue, nausea, and shortness of breath, which are easily misattributed to less serious conditions4.
Women May Experience ACS Differently
Women are more likely than men to present with atypical symptoms, leading to diagnostic challenges and delays in treatment5. For example, while men typically present with crushing chest pain during ACS, women may experience more atypical symptoms apart from chest pain such as:
- Fatigue: Feeling of an overwhelming sense of fatigue that is not relieved by rest.
- Dyspnoe: Experiencing shortness of breath, difficulty breathing or feel out of breath with minimal exertion.
- Nausea or Vomiting: Gastrointestinal symptoms such as nausea, vomiting, or indigestion are more commonly observed in women during ACS.
- Back or Jaw Pain: Pain can radiate to the back or jaw rather than the chest, leading to misinterpretation as musculoskeletal or dental issues.
- Dizziness or Lightheadedness: Feel dizzy or lightheaded, which can be mistakenly attributed to less serious conditions like dehydration or vertigo.
- Anxiety or Unusual Weakness: Feelings of anxiety or an unexplained sense of weakness can precede ACS.
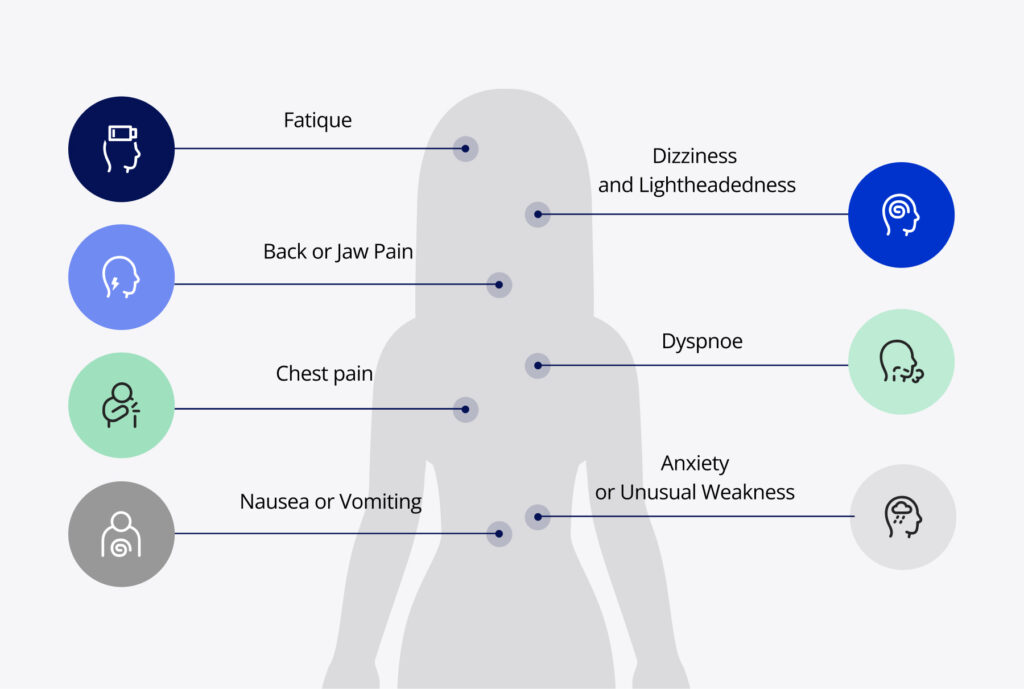
This clinical ambiguity highlights the need for heightened awareness and education among healthcare providers to recognize and respond to these non-classical presentations in women5.
It goes on
Biological Differences
Hormonal differences play a crucial role in how CVD manifest and progress in women compared to men. Estrogen, which has protective cardiovascular effects, significantly influences these differences, particularly during peri-menopause. Estrogen contributes to maintaining the vascular elasticity, improving blood flow, and reducing the likelihood of atherosclerosis. However, as women approach menopause and estrogen levels decline, their risk of developing CVD increases significantly6.
In addition to hormonal influences, women tend to have smaller coronary arteries than men, which can affect the presentation and detection of CVD. Smaller arteries are more challenging to visualize and treat during procedures such as coronary angiography and stenting. This anatomical difference can contribute to the underdiagnosis and undertreatment of ACS in women5.
Diagnostic Bias
Diagnostic bias significantly contributes to sex disparities in healthcare, often affecting clinical decision-making processes and resulting in women receiving less prompt and aggressive treatment compared to men7.
Studies have consistently shown that women experiencing ACS are less likely to receive evidence-based treatments and critical procedures12. For instance, women are less likely to be prescribed life-saving medications such as lipid-modifying agents, antiplatelet agents and ACE-inhibitors, and they are also less likely to undergo interventions such as angiography, angioplasty, and coronary artery bypass surgery 8,9,10,14.
Healthcare providers may unconsciously prioritize male patients for advanced diagnostic procedures and treatments, partly due to the traditional presentation of ACS symptoms that are more common in men.
There is a tendency to underestimate the severity of cardiovascular symptoms in women, leading to delays in seeking care and subsequent treatment. This delay can have grave consequences, as timely intervention is critical in improving outcomes for ACS patients8,13,14,15,16. Addressing this diagnostic bias requires ongoing education and awareness to recognize and respond to the unique presentation in women5.
Despite this awareness, progress in addressing these disparities has been slow.
What Can We Do About It?
To effectively address the sex disparities, it is essential to implement targeted strategies that provide women with the same quality and timeliness of care as men. Current research shows that women often experience longer “ECG-to-balloon” (E2B) and “door-to-balloon” (D2B) times compared to men, leading to delayed treatment and poorer outcomes11. For instance, women experiencing ACS may wait significantly longer for angiography and reperfusion therapy, which can be detrimental to their prognosis11.
Here are several steps you can take to help bridge this gap and improve care for female patients:
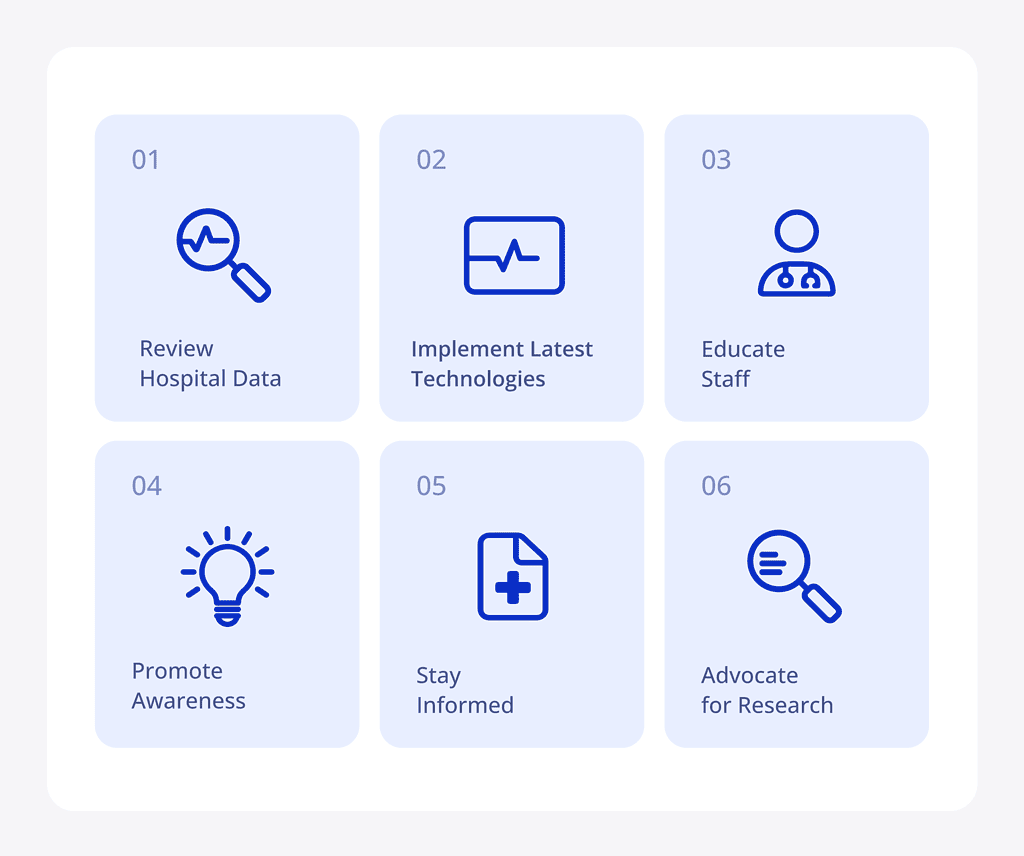
- Review Hospital Data: Analyze your hospital’s data to identify any sex disparities in treatment times and outcomes. Are women waiting longer for critical interventions at your institution? Identifying and understanding these gaps can help you target specific areas for enhancement.
- Educate Staff: Ensure that all healthcare providers in your facility are educated about the different ways ACS can present in women. This includes recognizing atypical symptoms such as fatigue, nausea, back pain, and shortness of breath, which are often overlooked or misattributed to less serious conditions. Emphasize the importance of early intervention and the unique risk factors women face. Regular training and updates on the latest research and guidelines can help keep staff informed and prepared.
- Advocate for Research: Support and participate in research studies that focus on understanding sex differences in CVD. Advocate for the inclusion of more women in clinical trials to guarantee that research findings are applicable to females too.
- Stay Informed: Keep yourself and your team updated on the latest research and guidelines on sex differences in cardiovascular care. Stay on top of the American Heart Association’s guidelines on heart disease in women and other articles that discuss the unique challenges they face in cardiovascular health12. Continuous learning will help you apply the most current and effective practices in your clinical setting.
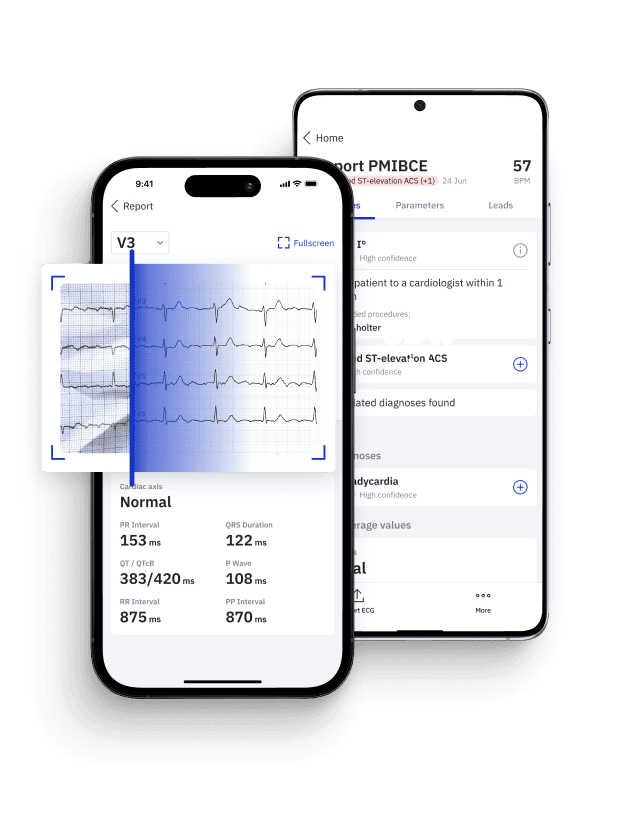
- Implement Latest Technologies: Integrate new diagnostic innovations into routine practice. The adoption of AI tools such as PMcardio can significantly reduce diagnostic delays and improve overall health outcomes, making it an essential strategy for any institution committed to healthcare equity. It is not swayed by stereotypes or historical biases, meaning it can provide objective assessments. This makes AI an indispensable tool in reducing disparities and advancing equitable healthcare practices.
- Promote Awareness: Increase awareness among your female patients about the unique risks and symptoms they might face. Encourage women to seek medical attention promptly if they experience symptoms, and educate them on the importance of not dismissing subtle signs of heart disease. Providing educational materials and hosting informational sessions within your community can help empower women to advocate for their health.
Actively closing the gap
Artificial intelligence holds significant potential in addressing disparities in healthcare by eliminating the biases that influence human decision-making. Tools like PMcardio can significantly improve the timely diagnosis of cardiac diseases by analyzing complex ECG patterns that human practitioners might miss. Importantly, PMcardio algorithms focus solely on the waveform itself, without being influenced by the patient’s age, sex or race, thereby providing unbiased and objective assessments. This ensures that high-risk patients are identified and treated promptly, regardless of demographic factors.17
The continuous learning capabilities of AI systems mean that they can adapt and improve over time as more data becomes available, further refining their diagnostic accuracy and effectiveness. This adaptability is vital in creating a more equitable healthcare environment where all patients receive timely and appropriate care. Implementing AI in clinical practice is a significant step towards bridging the diagnostic equity gap, ultimately leading to better health outcomes.

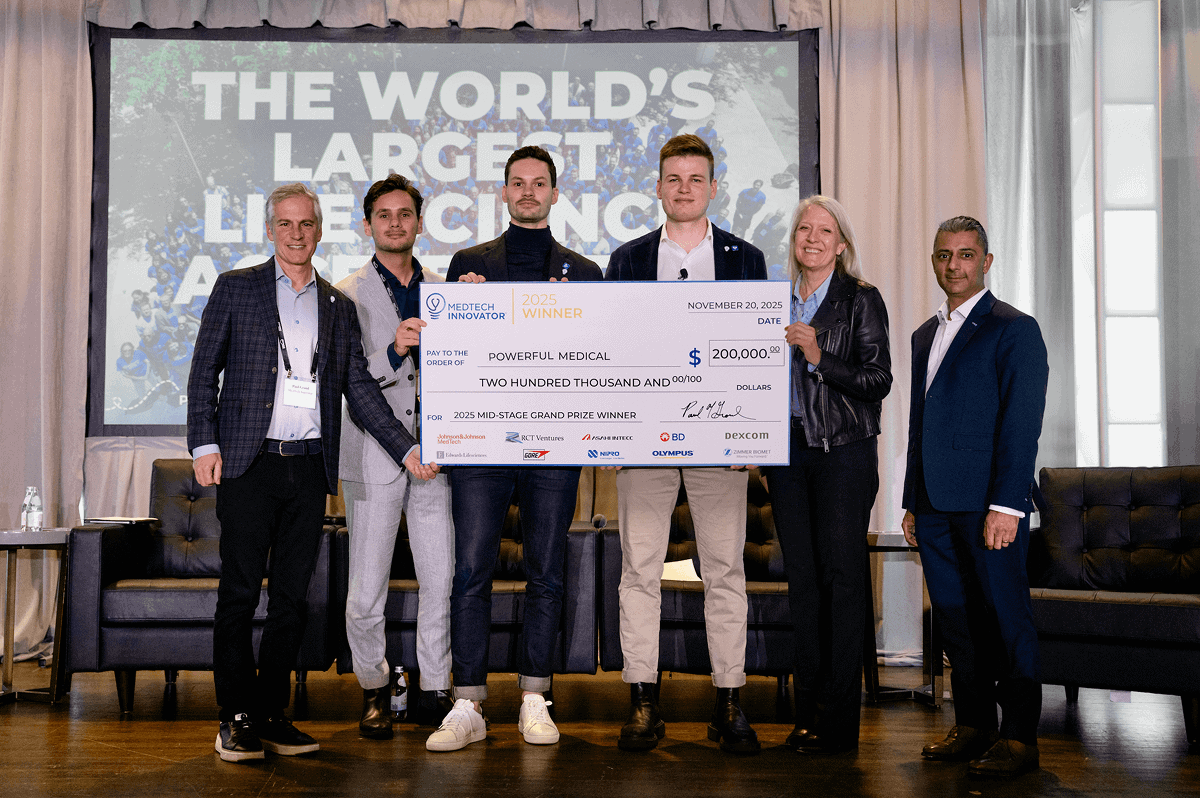
At Powerful Medical, we are actively conducting research into bias in diagnostic processes, focusing not only on sex bias but also on racial and ethnic biases, and working towards developing AI solutions that secure equitable care for all patients. Our commitment to this cause underscores the potential of technology to transform healthcare and reduce disparities.
Conclusion
Addressing sex disparities in cardiovascular care is an urgent and ongoing challenge. By understanding the unique ways that heart disease manifests in women and by implementing targeted strategies, healthcare providers can make significant strides in improving outcomes for female patients.
By leveraging the power of innovative technologies and a renewed focus on sex-specific healthcare, we can work towards a future where health outcomes are no longer influenced by sex. Through concerted efforts in education, research, and the implementation of unbiased diagnostic tools, we can ensure that women receive the equitable care they deserve.
Feeling Activated and Willing to Go Beyond? Please do!
With our innovative technologies and dedicated efforts, we are making strides toward true diagnostic equity through innovation. Contact our team at omi@powerfulmedical.com for guidance on how to effectively review and interpret your data to uncover valuable insights or if you would like to learn more about how AI can improve cardiovascular care for women at your institution.
References
- World Health Organization. Cardiovascular diseases (CVDs). [Internet]. 2021 [cited 2024 May 21]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- Gulati M. Why We Need Specialised Centres for Women’s Hearts: Changing the Face of Cardiovascular Care for Women. Circulation. 2020;141(7):592-595.
- Geller SE, Koch A, Pellettieri B, et al. Inclusion, analysis, and reporting of sex and race/ethnicity in clinical trials: have we made progress? J Womens Health (Larchmt). 2011;20(3):315-320.
- Mehta LS, Beckie TM, DeVon HA, et al. Acute Myocardial Infarction in Women. Circulation. 2016;133(9):916-947.
- Lichtman JH, Leifheit EC, Safdar B, et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: Evidence from the VIRGO study (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients). Circulation. 2018;137(8):781-790.
- Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American Heart Association. Circulation. 2011;123(11):1243-1262.
- Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, et al.; CRUSADE Investigators. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005 Mar 15;45(6):832-7. doi: 10.1016/j.jacc.2004.11.055. PMID: 15766815.
- Shaw LJ, Bugiardini R, Merz CN. Women and ischemic heart disease: evolving knowledge. J Am Coll Cardiol. 2009;54(17):1561-1575.
- Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353(7):671-682.
- Greenland P, Blaha MJ, Budoff MJ, et al. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72(4):434-447.
- Brush JE Jr, Chaudhry SI, Dreyer RP, D’Onofrio G, Greene EJ, Hajduk AM, et al. Sex Differences in Symptom Complexity and Door-to-Balloon Time in Patients With ST-Elevation Myocardial Infarction. Am J Cardiol. 2023 Jun 15;197:101-107. doi: 10.1016/j.amjcard.2023.03.009. Epub 2023 Apr 14. PMID: 37062667; PMCID: PMC10198892.
- American Heart Association. Heart Disease in Women. [Internet]. 2021 [cited 2024 May 21]. Available from: https://www.heart.org/en/health-topics/heart-attack/warning-signs-of-a-heart-attack
- Redfors B, Angerås O, Råmunddal T, Petursson P, Haraldsson I, Dworeck C, et al. Trends in Gender Differences in Cardiac Care and Outcome After Acute Myocardial Infarction in Western Sweden: A Report From the Swedish Web System for Enhancement of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART). J Am Heart Assoc. 2015 Jul 14;4(7):e001995. doi: 10.1161/JAHA.115.001995. PMID: 26175358; PMCID: PMC4608084.
- Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, et al.; CURE Investigators. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol. 2005 Nov 15;46(10):1845-51. doi: 10.1016/j.jacc.2005.05.091. Epub 2005 Oct 24. PMID: 16286169.
- Bugiardini R, Yan AT, Yan RT, Fitchett D, Langer A, Manfrini O, et al.; Canadian Acute Coronary Syndrome Registry I and II Investigators. Factors influencing underutilization of evidence-based therapies in women. Eur Heart J. 2011 Jun;32(11):1337-44. doi: 10.1093/eurheartj/ehr027. Epub 2011 Mar 7. PMID: 21383003.
- Cho L, Vest AR, O’Donoghue ML, Ogunniyi MO, Sarma AA, Denby KJ, et al.; Cardiovascular Disease in Women Committee Leadership Council. Increasing Participation of Women in Cardiovascular Trials: JACC Council Perspectives. J Am Coll Cardiol. 2021 Aug 17;78(7):737-751. doi: 10.1016/j.jacc.2021.06.022. PMID: 34384555.
- Powerful Medical. Powerful Medical Website. Available from: https://www.powerfulmedical.com/. Accessed May 21, 2024.