Occlusion Myocardial Infarction (OMI) refers to the acute occlusion or near-occlusion of a culprit coronary artery with insufficient collateral circulation, leading to transmural myocardial infarction and cardiac tissue death.
Unlike traditional diagnostic approaches, OMI is not defined solely by specific electrocardiographic (ECG) patterns, emphasizing the need for a comprehensive clinical assessment, including patient presentation, cardiac biomarkers like troponin, and coronary angiography findings.
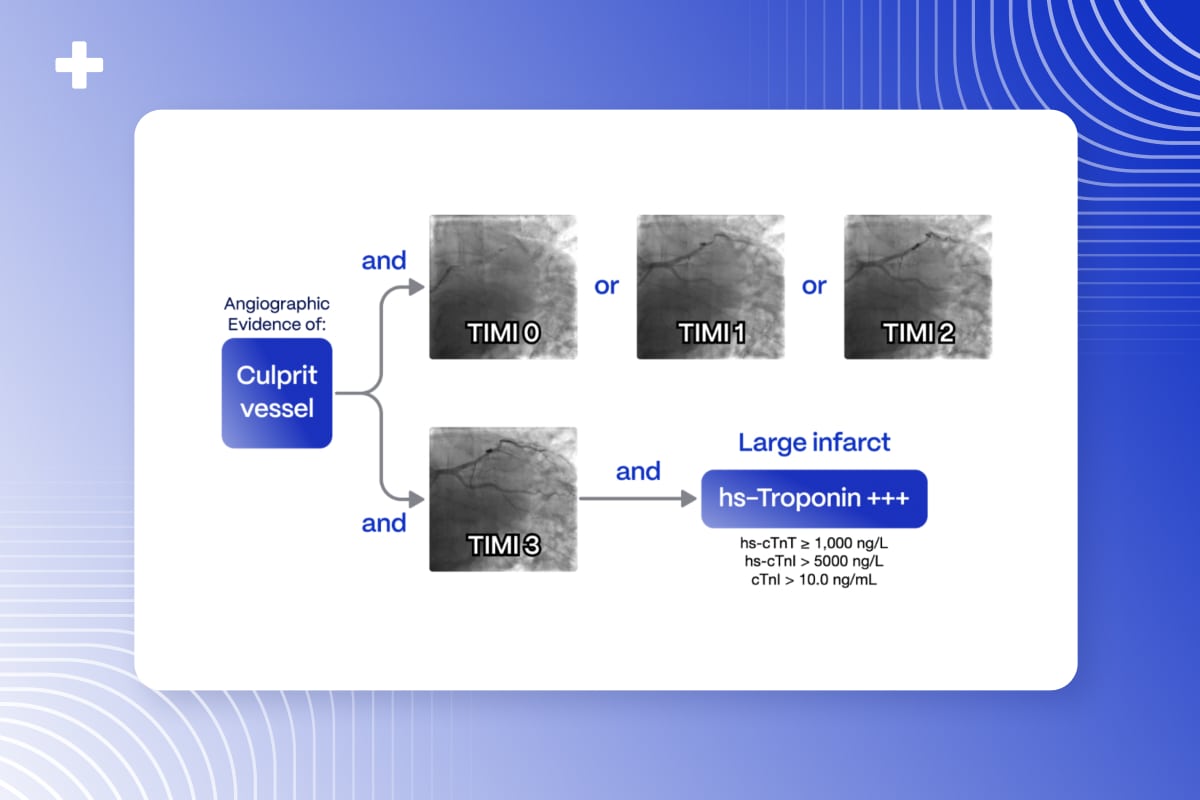
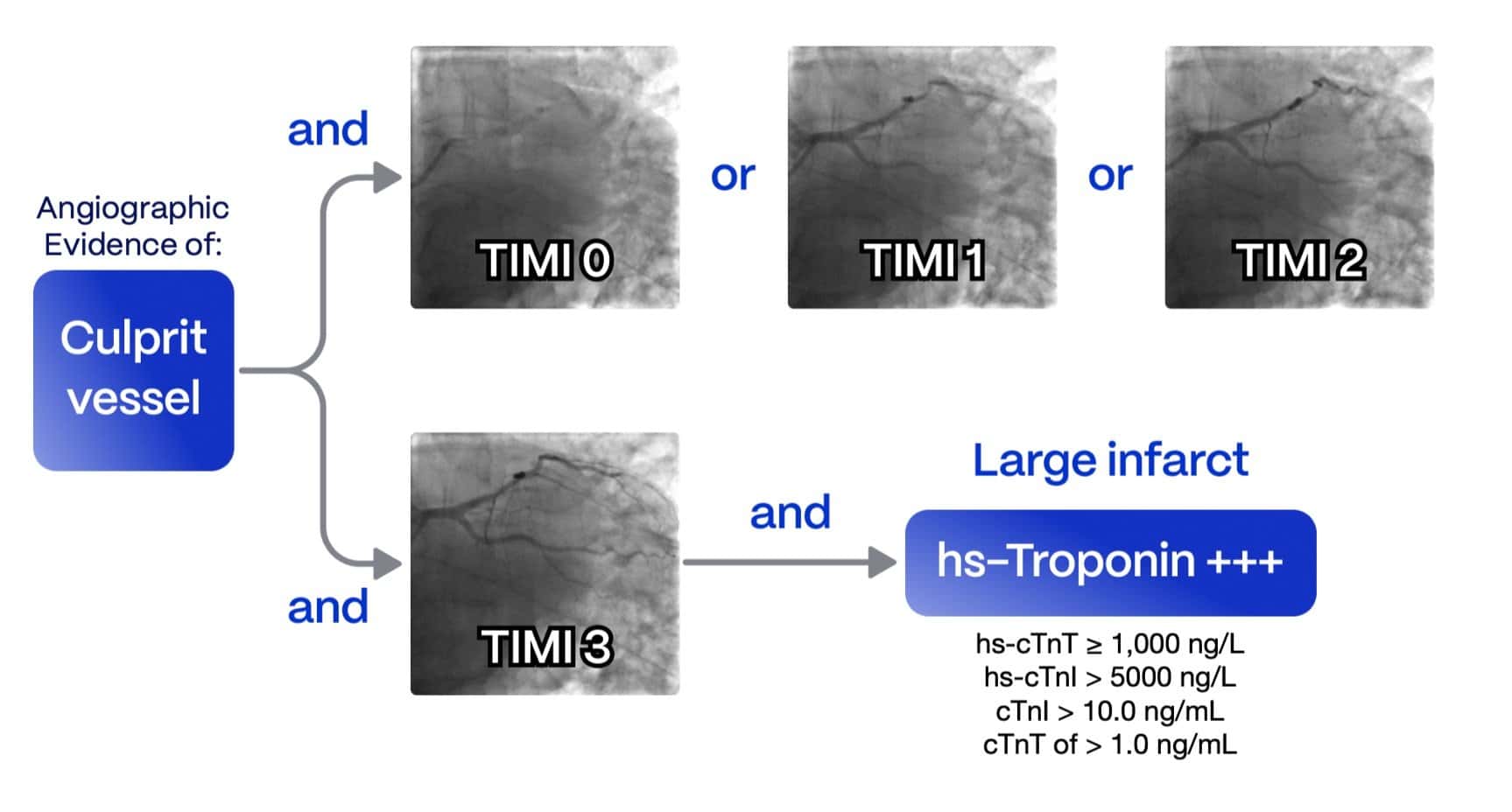
OMI is primarily identified through angiographic evidence, with endpoints including:
- TIMI 0-2 Flow in the culprit artery
- TIMI 3 Flow accompanied by high biomarker elevation, indicating a significant infarction caused by vessel occlusion.
This article explores the importance of early OMI identification, contrasts it with the STEMI criteria, and delves into the role of artificial intelligence (AI) in detecting OMI on a 12-lead ECG.
Table of Contents
The Need for Accurate and Early Diagnosis: ‘Time Is Muscle’
Chest pain remains the most common symptom among patients presenting to emergency departments, accounting for 15-20% of visits1. Rapid identification of OMI in these patients is crucial, as they require urgent therapy through percutaneous coronary intervention (PCI) to preserve cardiac tissue.
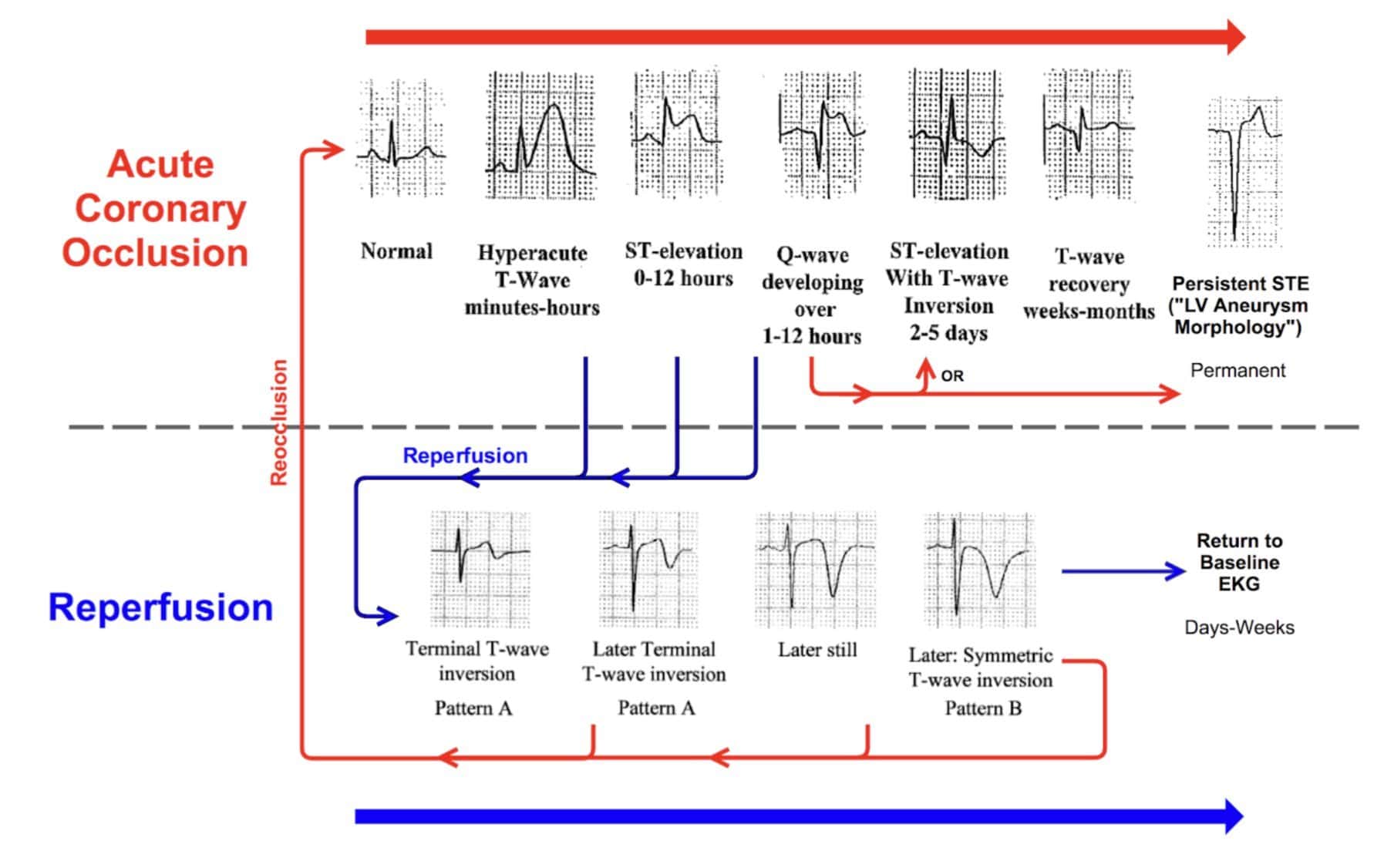
The ECG is widely available and facilitates quick initial patient stratification, traditionally based on ST-elevation myocardial infarction (STEMI) criteria. For over a decade, cardiology guidelines have relied on STEMI millimeter criteria to guide the need for emergent therapy2. However, increasing evidence suggests that STEMI criteria often fail to identify patients requiring immediate intervention3 accurately.
So what’s the problem with STEMI?
Acute coronary syndrome (ACS) encompasses dynamic ECG changes, complicating the identification of OMI using traditional STEMI criteria. Studies show that one-third of myocardial infarction patients without classic ST elevation are later found to have coronary occlusion upon angiography, leading to a significant delay in intervention and a twofold increase in patient mortality4.
Moreover, approximately 25% of emergency catheterization lab activations triggered by presumed STEMI turn out to be false positives, lacking a culprit vessel or elevated biomarkers5. These unnecessary activations strain healthcare resources and can cost over $10,000 per cath lab activation6.
From STEMI to OMI: The Paradigm Shift
The absence of STEMI criteria on an ECG does not eliminate the possibility of an occluded culprit vessel. In the new OMI paradigm, patients with ACS are assessed not only on ECG findings but also through clinical symptoms, biomarkers, and angiographic results. This paradigm divides patients into:
- Occlusion Myocardial Infarction (OMI): Near or complete occlusion of a culprit vessel with inadequate collateral support, leading to active infarction.
- Non-Occlusion Myocardial Infarction (NOMI): Absence of occlusion or sufficient collateral support, preventing active infarction, which includes but is not limited to MINOCA cases.
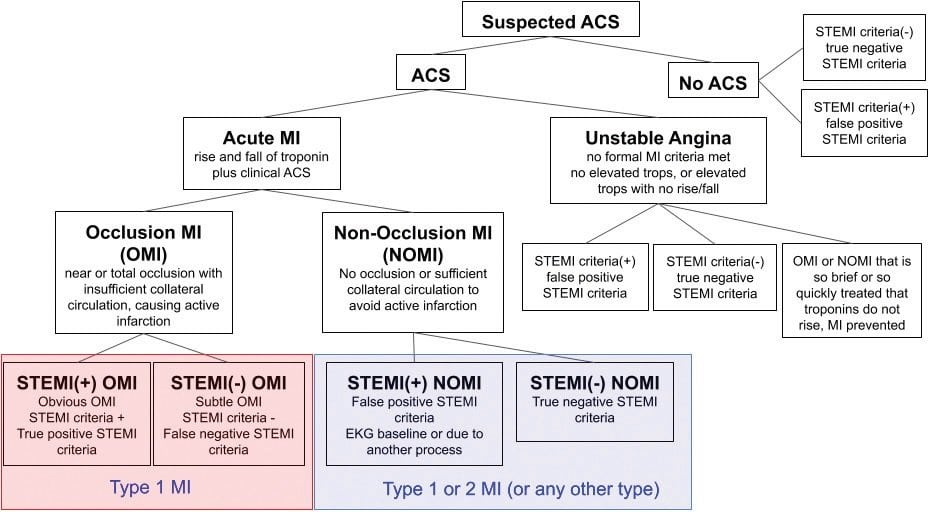
This approach enables the identification of patients with angiographic occlusion, even in the absence of typical ST elevation.
Unlike the previous paradigm, we can now accurately identify patients without typical ST-elevation on their initial ECG but with thrombotic occlusion of the mid-left circumflex artery (mLCx), causing subtle ST depression in V3 as OMI.
OMI ECG Criteria: Recognizing Subtle Patterns
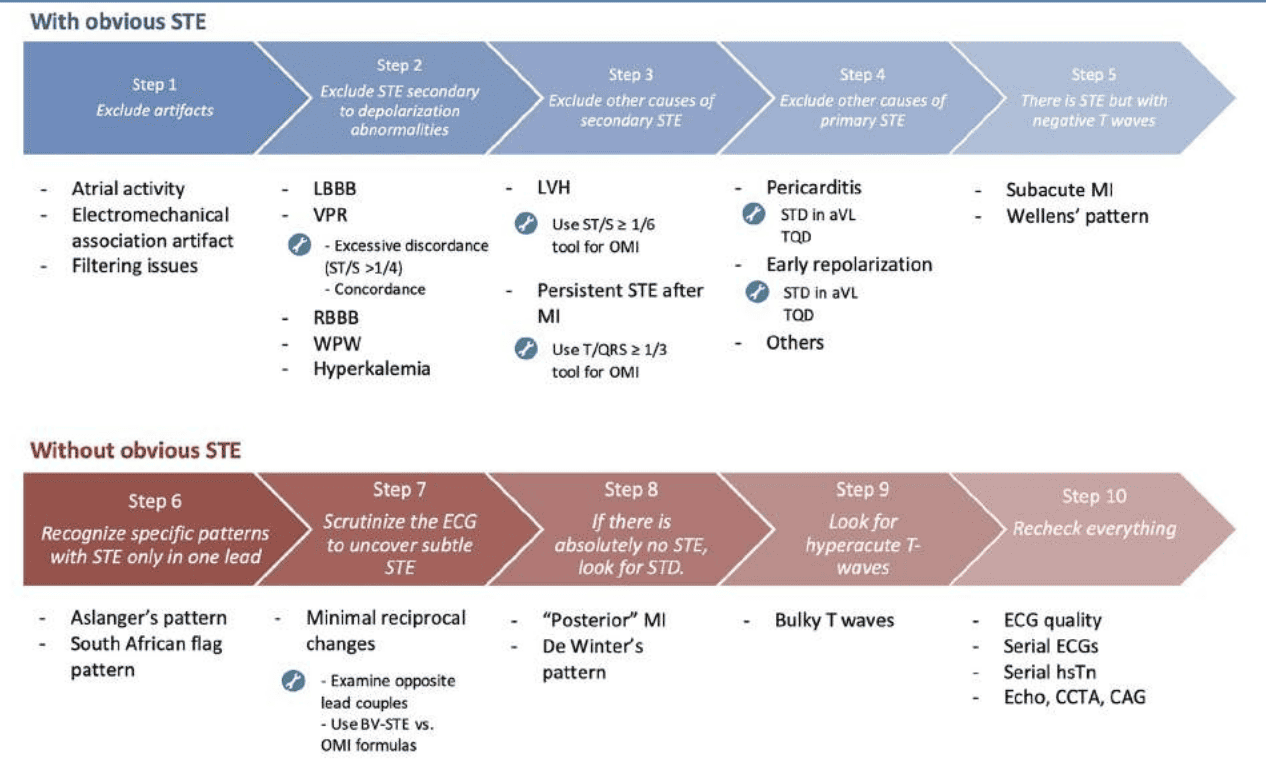
While ST elevation may be absent in nearly half of OMI cases, specific ECG findings can indicate an occluded vessel. The OMI paradigm does not rely on millimeter criteria but instead emphasizes careful examination of the ECG and clinical context. Dr. Emre Aslanger has developed a flowchart illustrating OMI identification on ECG, highlighting key features such as:
- ST elevation in a single lead
- Subtle ST elevation with minimal reciprocal changes
- Isolated ST depression
- Prominent (hyperacute) T-waves7
Increasing evidence shows that relying on STEMI criteria frequently fails to identify patients who require immediate invasive management accurately. The 2022 American College of Cardiology Chest Pain Expert Consensus³ has recently acknowledged the limitations of STEMI criteria and defined new STEMI equivalents.
STEMI Equivalents: Navigating Hidden Indicators of Acute Coronary Occlusion
Recognizing these STEMI equivalents is critical, as they represent high-risk occlusions that may otherwise be missed with standard STEMI criteria. This nuanced understanding allows clinicians to detect occlusions that traditional criteria might overlook.
Accuracy of OMI ECG criteria
A study involving 808 patients with acute coronary syndrome confirmed that using OMI-specific ECG interpretation significantly increases diagnostic sensitivity, raising it from 41 % with traditional STEMI criteria to 86 %, while maintaining a comparable specificity of 91% vs. 94% respectively.
These findings highlight the effectiveness of OMI criteria in accurately diagnosing occlusion myocardial infarction and underscore the importance of timely intervention to improve patient outcomes.
The Role of AI in OMI Detection
Accurate OMI diagnosis demands a nuanced understanding of complex ECG patterns, a skill that expert clinicians acquire through extensive experience. Equipping healthcare providers with this expertise can be challenging, but artificial intelligence offers a transformative solution.
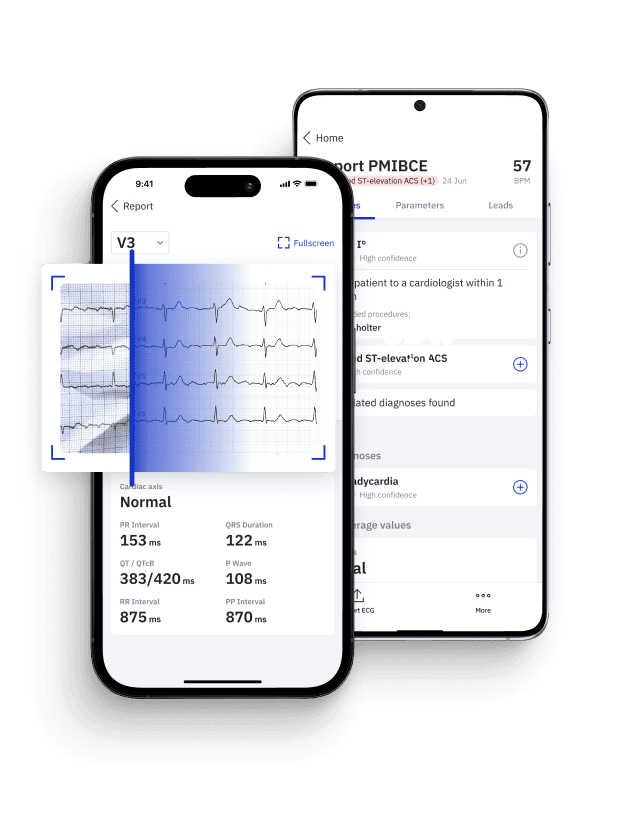
European Heart Journal: Clinical Validation Study of the PMcardio OMI AI Model
Affectionately known as the Queen of Hearts, PMcardio is trained on extensive datasets of angiographically confirmed OMI ECGs. By leveraging deep learning, it empowers clinicians to identify OMI with high precision, significantly enhancing diagnostic accuracy and facilitating prompt, effective patient care.
Conclusion
The shift from STEMI to OMI paradigm represents a significant advancement in the management of acute myocardial infarction, acknowledging the limitations of traditional ECG-based STEMI criteria. By integrating clinical context, biomarkers, and advanced ECG interpretation criteria such as STEMI equivalents, the OMI paradigm allows for more accurate diagnosis and timely intervention. AI-powered tools are likely to enhance this paradigm shift further, enabling broader adoption and supporting clinicians in early and precise OMI detection.
FAQ: Occlusion Myocardial Infarction (OMI)
What is an Occlusion Myocardial Infarction?
OMI, or Occlusion Myocardial Infarction, refers to a type of myocardial infarction resulting from a complete or near-complete coronary artery occlusion, leading to myocardial tissue necrosis. Unlike STEMI, OMI does not always present with classic ECG changes, often necessitating advanced diagnostic methods and nuanced ECG interpretation to identify high-risk occlusions accurately.
Is an occlusion a complete blockage?
Yes, in the context of myocardial infarction, occlusion denotes a complete or near-complete obstruction of a coronary artery, resulting in significantly diminished or absent blood flow to the affected myocardial tissue. This ischemic event rapidly progresses to myocardial necrosis if revascularization is not achieved promptly.
How accurate are OMI ECG findings vs. STEMI?
OMI ECG criteria have demonstrated significantly higher sensitivity in detecting coronary occlusions than traditional STEMI criteria. Studies indicate that OMI criteria can identify up to 86% of occlusion cases, nearly double the 41% sensitivity seen with STEMI criteria, while maintaining comparable specificity. This enhanced accuracy underscores the utility of OMI criteria in identifying high-risk patients who may otherwise be missed.
Why do occlusions rapidly lead to infarction in the heart?
Coronary occlusions obstruct oxygenated blood flow to the myocardium, leading to ischemia and, if unresolved, infarction. Cardiomyocytes begin to undergo irreversible damage within approximately 90 minutes of sustained ischemia, with necrosis progressing rapidly thereafter. Prompt intervention to restore perfusion within this critical window is essential to minimize myocardial injury and preserve cardiac function.
How does OMI manifest on an ECG?
OMI on ECG can present with subtle findings, including minor ST-elevations, isolated ST-depressions, or hyperacute T-waves, which are often considered STEMI equivalents. Unlike STEMI, OMI does not always display prominent ST-segment elevation, making interpretation more challenging. Recognizing these STEMI equivalents is essential, as they indicate high-risk occlusions that may otherwise be missed with standard STEMI criteria. This subtlety often necessitates a comprehensive assessment, combining clinical context and advanced diagnostic methods to accurately identify and manage occlusions effectively.
Pin Down Occlusive MI with Certified AI
- Medical Device Class II(b) EU MDR CE-mark
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- 5 FREE ECGs/month - no credit card needed
References
- Ekelund U;Akbarzadeh M;Khoshnood A;Björk J;Ohlsson M; (2012, August 8). Likelihood of acute coronary syndrome in emergency department chest pain patients varies with time of presentation. BMC research notes. https://pubmed.ncbi.nlm.nih.gov/22871081/
- Ibanez B;James S;Agewall S;Antunes MJ;Bucciarelli-Ducci C;Bueno H;Caforio ALP;Crea F;Goudevenos JA;Halvorsen S;Hindricks G;Kastrati A;Lenzen MJ;Prescott E;Roffi M;Valgimigli M;Varenhorst C;Vranckx P;Widimský P; ; (2018, January 7). 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with st-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with st-segment elevation of the European Society of Cardiology (ESC). European heart journal. https://pubmed.ncbi.nlm.nih.gov/28886621/
- Kontos, M. C., De Lemos, J. A., Deitelzweig, S., Diercks, D. B., Gore, M. O., Hess, E. P., McCarthy, C. P., McCord, J., Musey, P. I., Villines, T. C., & Wright, L. J. (2022). 2022 ACC Expert Consensus Decision Pathway on the evaluation and disposition of acute chest pain in the Emergency Department. Journal of the American College of Cardiology, 80(20), 1925–1960. https://doi.org/10.1016/j.jacc.2022.08.750
- Khan, A. R., Golwala, H., Tripathi, A., Abdulhak, A. a. B., Bavishi, C., Riaz, H., Mallipedi, V., Pandey, A., & Bhatt, D. L. (2017). Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. European Heart Journal, 38(41), 3082–3089. https://doi.org/10.1093/eurheartj/ehx418
- McCabe, J. M., Armstrong, E. J., Kulkarni, A., Hoffmayer, K. S., Bhave, P. D., Garg, S., Patel, A., MacGregor, J. S., Hsue, P. Y., Stein, J. C., Kinlay, S., & Ganz, P. A. (2012). Prevalence and factors associated with False-Positive ST-Segment Elevation myocardial infarction diagnoses at Primary Percutaneous Coronary Intervention–Capable Centers. Archives of Internal Medicine, 172(11). https://doi.org/10.1001/archinternmed.2012.945
- Degheim, G., Berry, A., & Zughaib, M. (2019). False activation of the cardiac catheterization laboratory: The price to pay for shorter treatment delay. JRSM Cardiovascular Diseases, 8, 204800401983636. https://doi.org/10.1177/2048004019836365
- Aslanger, E., Meyers, H. P., & Smith, S. W. (2021). Recognizing electrocardiographically subtle occlusion myocardial infarction and differentiating it from mimics: Ten steps to or away from cath lab. Turk Kardiyoloji Dernegi Arsivi-Archives of the Turkish Society of Cardiology, 49(6), 488–500. https://doi.org/10.5543/tkda.2021.21026
- Meyers, H. P., Bracey, A., Lee, D., Lichtenheld, A., Li, W. J., Singer, D., Rollins, Z., Kane, J., Dodd, K. W., Meyers, K., Shroff, G. R., Singer, A. J., & Smith, S. W. (2021). Accuracy of OMI ECG findings versus STEMI criteria for diagnosis of acute coronary occlusion myocardial infarction. IJC Heart & Vasculature, 33, 100767. https://doi.org/10.1016/j.ijcha.2021.100767