Introduction
ST-Elevation Myocardial Infarction (STEMI) is a critical, life-threatening condition that requires immediate recognition and intervention to reduce morbidity and mortality. Understanding the ECG criteria for diagnosing STEMI is crucial for clinicians, as it enables rapid decision-making in emergency situations.
This article will guide healthcare professionals through the essential STEMI ECG criteria, address the evolving understanding of STEMI equivalents, and discuss the growing role of artificial intelligence (AI) in supporting clinical practice.
Table of Contents
What is a STEMI?
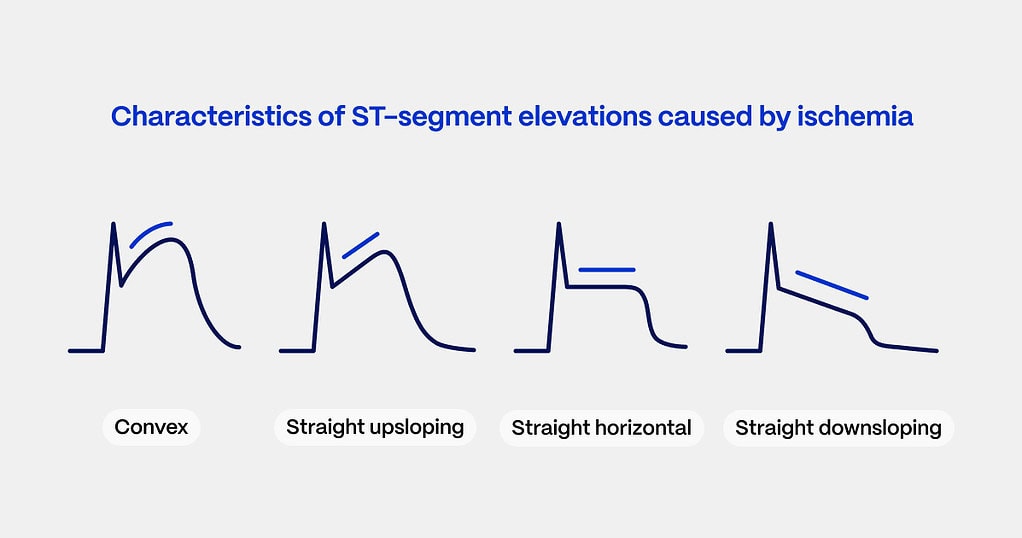
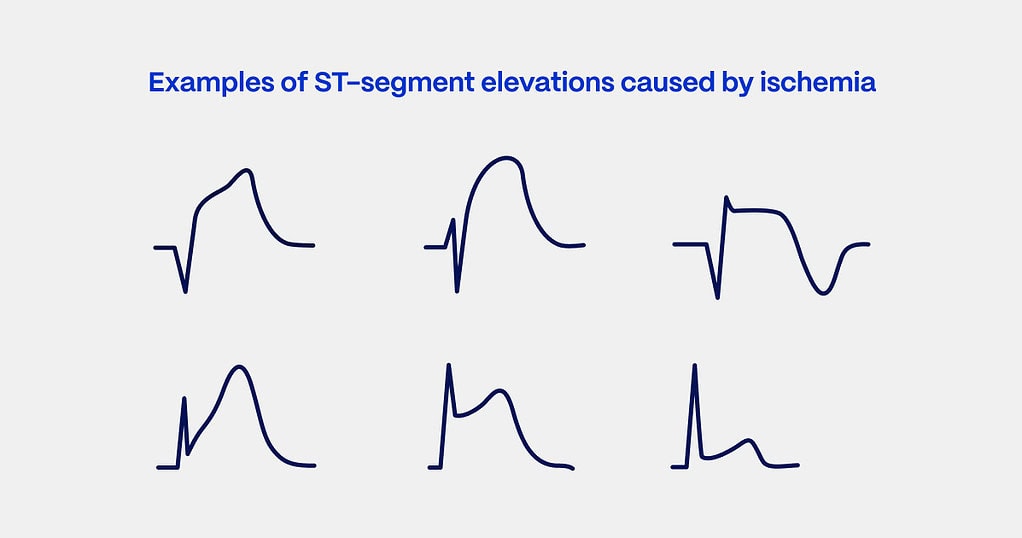
STEMI, or ST-Elevation Myocardial Infarction, is a severe form of acute coronary syndrome (ACS), typically caused by the complete occlusion of a coronary artery, leading to significant myocardial damage2. The hallmark of STEMI is ST-segment elevation on a 12-lead ECG, which signifies transmural infarction – damage involving the full thickness of the myocardium2.
Prompt recognition and intervention are vital to preserving cardiac function and reducing the risk of complications such as heart failure and sudden cardiac death3.
Pathophysiology of STEMI
STEMI occurs when an atherosclerotic plaque within a coronary artery ruptures, resulting in the formation of a thrombus that obstructs blood flow4. The ischemia that follows leads to myocardial necrosis, a process reflected in specific ECG changes4. Recognizing these changes is key to initiating timely reperfusion therapies such as percutaneous coronary intervention (PCI)5.
The extent and location of the infarction influence both clinical symptoms and ECG findings as ischemia progresses from subendocardial to transmural infarction5.
Key STEMI ECG Criteria
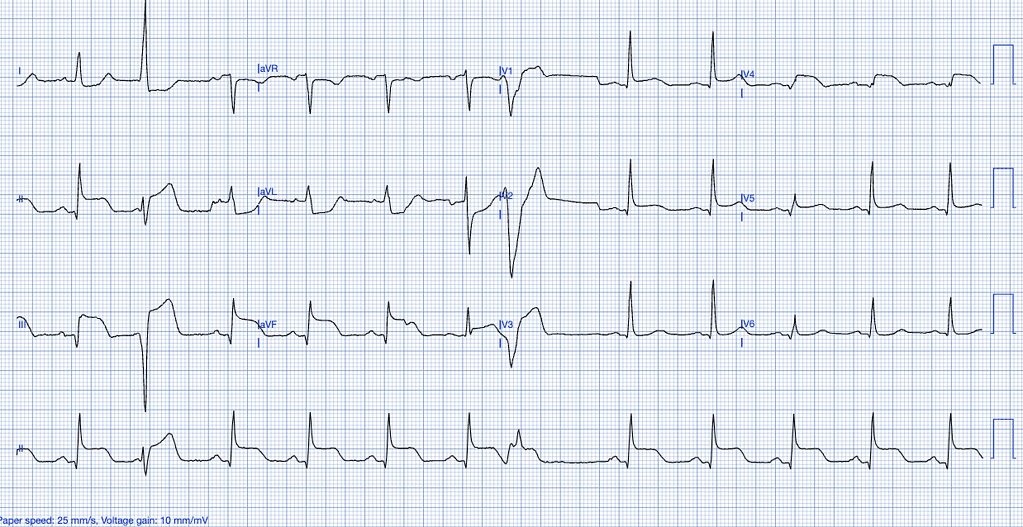
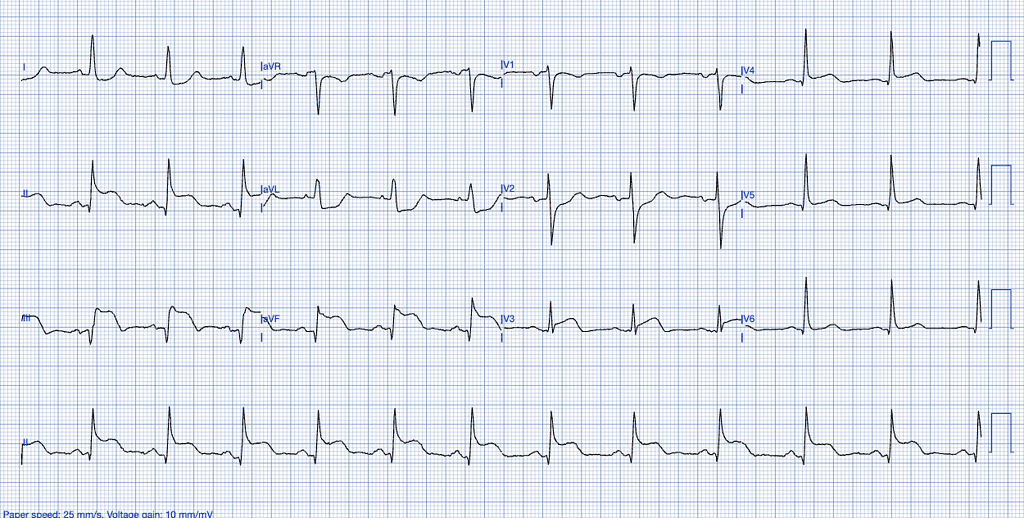
The primary diagnostic tool for identifying STEMI is the 12-lead electrocardiogram (ECG). As a dynamic diagnostic tool, the ECG captures the heart’s electrical activity at a specific moment in time and serves primarily as a “rule-in” test for STEMI6. However, an initial absence of ST-segment elevation does not entirely rule out serious coronary pathology, as ischemic patterns can evolve6.
To accurately diagnose a STEMI, clinicians must be familiar with the following ECG criteria7:
| Lead Group | ST-Elevation Threshold |
|---|---|
| Limb Leads (I, II, III, aVL, aVF) | ≥1 mm (0.1 mV) of ST-segment elevation in two or more contiguous leads |
| Chest Leads (V1-V6) | ≥1 mm of ST-segment elevation in two or more contiguous leads, except for V2 and V3 |
| Anterior Leads (V2-V3) | Men < 40 years: ≥2.5 mm Men ≥ 40 years: ≥2 mm Women (any age): ≥1.5 mm |
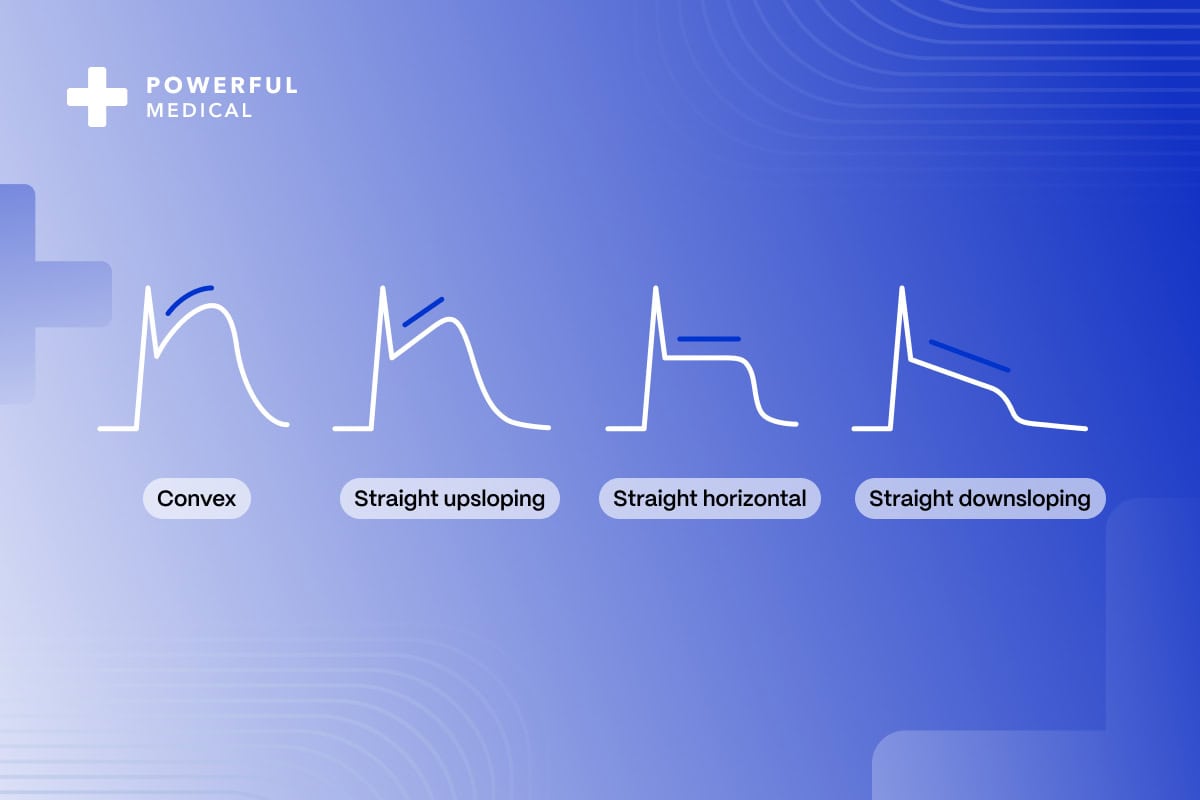
For accurate measurement, the ST-segment elevation should be assessed 0.04 seconds after the J-point, the junction where the QRS complex ends and the ST segment begins7. Misinterpretation of this measurement could lead to incorrect diagnoses, especially in cases of STEMI mimics in conditions such as early repolarization, (myo)pericarditis and others8.
STEMI and Its Limitations: Recognizing Other Myocardial Infarction Patterns
STEMI is defined by characteristic ST-segment elevation on an ECG, but not all life-threatening myocardial infarctions (MIs) present with this pattern9. Some patients experience coronary occlusions that don’t meet the classical STEMI ECG criteria yet still warrant urgent intervention.
These cases, often referred to as STEMI equivalents, include patterns such as de Winter’s T-waves, Sgarbossa Criteria, hyperacute T waves, South African flag sign and others10.
- Hyperacute T-Waves: A Comprehensive Pattern Exploration
- Sgarbossa Criteria: A Gateway to Advanced Cardiac Diagnosis
- Wellens’ Syndrome: Are You Prepared to Prevent Acute Coronary Occlusions?
Recognizing these STEMI equivalents is critical, as missing such patterns can delay diagnosis and treatment, leading to worsened patient outcomes11. Clinicians must be aware of these atypical presentations, which often do not exhibit classic ST-segment elevation but indicate a need for urgent reperfusion therapy12.
STEMI Mimics: The Hidden Impostors of Myocardial Infarction
In addition to STEMI equivalents, clinicians must be vigilant about STEMI mimics – conditions that resemble STEMI on an ECG but are not due to acute coronary occlusions. Common examples include early repolarization, (myo)pericarditis, and left ventricular hypertrophy, which can lead to false-positive diagnoses and unnecessary interventions.
Accurate interpretation of these patterns is crucial to prevent misdiagnoses and ensure that only genuine cases of coronary occlusion are prioritized for immediate reperfusion therapy13.
The Evolution of STEMI Diagnosis
Recent updates to the European Society of Cardiology (ESC) guidelines on acute coronary syndromes emphasize a broader spectrum of myocardial infarction presentations13. With the increasing recognition of STEMI equivalents, clinicians are urged to stay informed about emerging ECG patterns that signal life-threatening coronary occlusions, even when ST-segment elevation is absent.
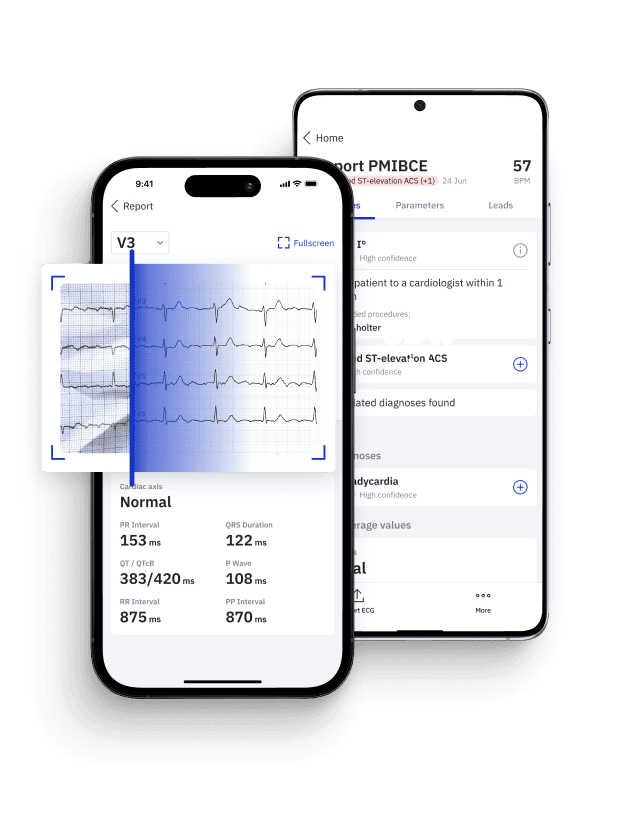
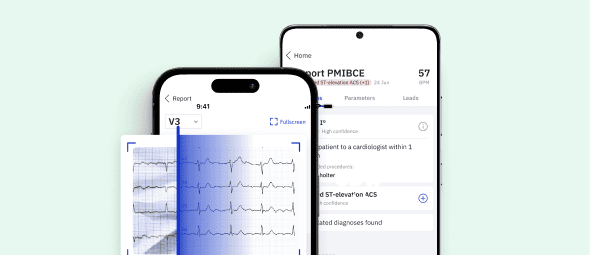
Given the rapid influx of new clinical data, it can be challenging to stay updated on all possible STEMI presentations. AI-driven technologies, such as PMcardio, offer valuable support by providing real-time, accurate identification of both STEMI and its equivalents.
This ensures that even subtle ECG changes, which may be overlooked in a busy clinical environment, are recognized promptly, leading to faster interventions14 and better patient outcomes.
AI’s Role in STEMI Diagnosis
The use of AI in clinical practice, particularly for ECG interpretation, is transforming how STEMI and its equivalents are detected. Tools like PMcardio leverage deep learning algorithms to analyze ECGs in real time, reducing the likelihood of human error14.
By recognizing complex patterns or subtle deviations that could indicate a coronary event, AI can augment clinical decision-making in chest pain patient cohorts, leading to improved patient triage and appropriate and timely cath lab activations15.
Pin Down Occlusive MI with Certified AI
- Medical Device Class II(b) EU MDR CE-mark
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- 5 FREE ECGs/month - no credit card needed
Conclusion
Understanding and accurately identifying STEMI ECG criteria is fundamental for healthcare professionals involved in emergency cardiac care. As our understanding of MI evolves, especially with the recognition of STEMI equivalents, tools like PMcardio can play a crucial role in supporting clinicians. By incorporating AI technology, healthcare providers can enhance diagnostic accuracy, stay ahead of emerging clinical challenges, and ultimately improve outcomes for patients experiencing ACS15.
References
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2013;61(4)
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231-2264.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes. J Am Coll Cardiol. 2014;64(24)
- Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368(21):2004-2013.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39(2):119-177.
- Alpert JS, Thygesen K, Antman E, et al. Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee. J Am Coll Cardiol. 2000;36(3):959-969.
- Birnbaum Y, Bayes de Luna A, Fiol M, et al. Common pitfalls in the interpretation of electrocardiograms from patients with acute coronary syndromes with narrow QRS: a consensus report. J Electrocardiol. 2014;47(5):462-475.
- Smith SW, Khalil K, Henry TD, et al. Electrocardiographic Differentiation of Early Repolarization and Acute Myocardial Infarction in the Emergency Department. Ann Emerg Med. 2012;60(1):45-56.
- de Winter RJ, Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359(19):2071-2073.
- Brady WJ, de Winter RJ. The electrocardiographic T wave: physiological, pathophysiological, and therapeutic considerations. J Emerg Med. 2013;45(2):329-337.
- Wang K, Asinger RW, Marriott HJL. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003;349(22):2128-2135.
- Macfarlane PW, et al. The Early Repolarization Pattern: A Consensus Paper. J Am Coll Cardiol. 2015;66(4):470-477.
- Moak JH, Muck AE, Brady WJ. ST-segment elevation myocardial infarction mimics: The differential diagnosis of nonacute coronary syndrome causes of ST-segment/T-wave abnormalities in the chest pain patient. Turk J Emerg Med. 2024;24(4):206-217.
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289-1367.
- Herman R, Meyers HP, Smith SW, Bertolone DT, Leone A, Bermpeis K, et al. International evaluation of an artificial intelligence-powered electrocardiogram model detecting acute coronary occlusion myocardial infarction. Eur Heart J Digit Health. 2023;5(2):123-33. doi:10.1093/ehjdh/ztad074.
- Powerful Medical. PMcardio for organizations: AI-powered ECG interpretation. Powerful Medical [Internet]. 2023 [cited 2024 Sep 24]. Available from: https://www.powerfulmedical.com/pmcardio-organizations/