Our Chief Medical Officer, Dr Robert Herman, was recently a guest on Mayo Clinic’s Cardiovascular CME Podcast, with the topic of “AI-Augmented ECG Interpretation Using Smartphone Technology.” The podcast host, Anthony H. Kashou, MD, asked Robert Herman how we at Powerful Medical unlock the full potential of any paper ECG using AI.
You can listen to the podcast here or read the main takeaways below.
Our CMO, Robert Herman, MD, discusses the future roadmap for leveraging the AI ECG interpretation on the Mayo Clinic podcast.
Main topics discussed:
- What is AI-powered ECG digitisation, and how does it work?
- What are the current challenges of automated ECG interpretation?
- What’s next for the AI-powered ECG, and how can we unlock its full potential?
Introduction:
Electrocardiogram remains critical to clinical practice. With the advent of new artificial intelligence-augmented ECG algorithms, we are witnessing exciting advances in electrocardiography. These developments have the potential to improve cardiovascular care in the clinical workflow. In this episode of the Mayo Clinic’s podcast, Anthony and Robert discuss an interpretation of ECGs using smartphone technology, existing challenges in automated ECG interpretation, and AI’s future in electrocardiography.
Anthony: Robert, you and your team have developed an AI-powered ECG digitisation and interpretation tool. How does it work?
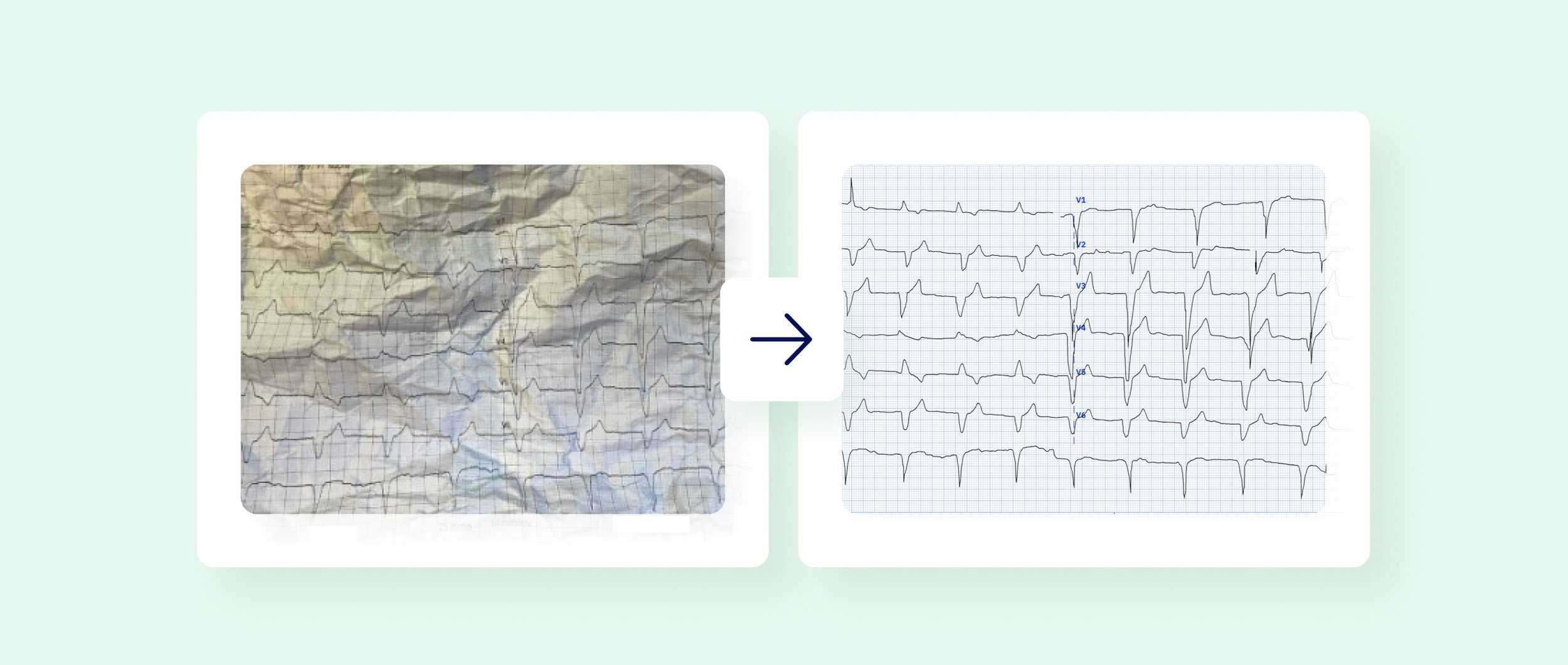
Robert: Our AI ECG digitisation application PMcardio can digitise and standardise any image of any 12-lead ECG. How it works is that a healthcare professional would take a picture of an ECG of any format or manufacturer. PMcardio will then convert it to a fully digital ECG waveform while maintaining the original sampling frequency of the ECG – as if it was coming out of an ECG machine.
We can process any ECG – even one that has been damaged, messy, old, etc. Our app can process and standardise any paper crumples on the ECG or remove coffee stains or scribbles. Therefore, we are not limited to high-quality ECG scans as input.
PMcardio converts any image of any ECG to a fully digital ECG and then processes it further – interprets an ECG like a human cardiologist would. Our AI algorithms detect up to 38 cardiac abnormalities on the ECG. We do the basic rhythm analysis and the arrhythmias and detect infarctions and heart blocks.
PMcardio is a fully certified medical device. The biggest added value of PMcardio is that it does not stop at a diagnosis. The app puts the clinical diagnosis into the clinical context of the patient, tackling the fact that the clinical context has a lot of weight in diagnosing the patient and deciding the next step. Our algorithms combine the diagnosis with the symptom checker that gathers the clinical context (the patient’s clinical parameters) and outputs the decision for referral and further diagnostic and treatment procedures.
Anthony: What was the validation process of your app?
Robert: Validation is critical when working with AI. We have validated PMcardio on the most extensive data set of over 12,000 ECG test cases. We have also benchmarked PMcardio by comparing it to the current state-of-the-art. For us, it’s represented by general practitioners (family physicians) and cardiologists. In this validation, we were able to demonstrate a statistical superiority over non-cardiologist HCPs, and we were able to show that PMcardio is non-inferior to cardiologists in all of the diagnoses across the board. Our medical device has improved arrhythmia and acute MI detection compared to the state-of-the-art.
In 2022, we also ran one of the largest randomised controlled clinical trials, trialling cardiac AI software with two health insurance companies in Europe and 58 participating primary care centres, where we enrolled more than 800 patients. We’re currently analysing the results, but what we know so far is that there is a high adherence rate towards what PMcardio has recommended in the intervention. We are now analysing the other endpoints, such as the percentage of adequately referred patients in the intervention group compared to the control group and other health-economic endpoints that quantify the costs of inadequately referred patients.
Anthony: What do you see as the current challenges of automated ECG interpretation? And how do we tackle them?
Robert: I would summarise the current challenges in the ECG interpretation space in four major points.
1. There is a lack of standardisation in electrocardiography, which is evident in many domains in the medical field.
ECG interpretation is still quite subjective, and there is little consensus, for example, with Left Bundle Branch Block criteria or the diagnosis of LVH from an ECG. If you doubt this, just look at the comment section on Twitter or Facebook, where people post ECG cases quite frequently. Some of these conversations get really heated, and there is little consensus, especially on the odd-looking ECGs that are not as clear as in a picture book.
2. The non-AI solutions that computerise the electrocardiogram are very susceptible to noise.
We see that with the existing algorithms where if the naturally occurring noise that usually occurs in the clinic, like high-frequency noise when the waveform is fuzzy, or when the base side of the waveform wonders, these non-AI solutions are very susceptible to that, and these minor noise artefacts can trick the interpretation algorithm.
3. ECG interpretation is not only dependent on the ECG waveform itself but can be very dependent on clinical parameters such as age, gender, or the patient’s symptoms.
These parameters have a massive influence on the resulting diagnosis but also on the triage and management of the patient. For example, a classic case is an incidental finding of the Right Bundle Branch Block or the Right Bundle Branch Block in the context of an Acute right heart strain during the Pulmonary Embolism. Those are two different things that have two different levels of importance. However, you can only figure that out once you add the patient’s clinical parameters to the picture.
4. Even though there’s a lot of publicly available ECG data, these data sets are frequently inaccurate and not large enough to train and validate a model.
Anthony: What’s next for AI-powered ECG? How can we unlock its full potential?
Robert: There is a lot of exciting research in this space. At Powerful Medical, we always try to unlock more from the ECG. ECG is currently the primary input that we process within the company. There are three ways I see AI-powered ECG evolving in the next couple of years.
1. We will move away from training on subjective interpretations to training and evaluating our models on objective outcome parameters such as angiographic results or echocardiographic parameters.
We see an influx in this space and a lot of work pioneered by the Mayo Clinic, and we’re also active here. We have recently worked with Dr Steven Smith and Dr Pendell Meyers on an algorithm detecting even subtler acute coronary occlusion. We validated this algorithm on the EU and US cohorts. We were able to increase quite notably the sensitivity of detecting acute coronary occlusion while maintaining the specificity of the STEMI criteria – improving the diagnosis of acute heart attack patients, which means we can detect these patients hours earlier than the STEMI criteria and send them accordingly to the cath lab. We have a study coming out very soon, and we also focus on other areas, such as heart failure, EP, and sudden cardiac death, rolling out shortly after this ACS module.
2. Also, we will see improvement in predictive capabilities.
We’re working on predicting the risk of these acute events occurring and analysing ECGs consecutively in time to see who will develop this acute event and prevent it from happening.
3. With the advances in AI, what will be interesting is the processing of the raw ECG data itself.
Due to the limited human capabilities, we have filters on the ECG devices and hardware filters that filter the waveform. We do that because the human eye cannot process such a messy waveform as found in the raw ECG data. But thanks to AI, we can look at these raw signals. This could be the key to unlocking more context from the ECG and enabling even more complex topics, such as an in-depth analysis of the P-waves or trying to predict precursors to atrial fibrillation.
Stay on the pulse with our newsletter
Your submission was successful
To close things up
The ECG remains an essential aspect of patient care, and while we continue to witness advances in electrocardiography, there are still challenges with automated ECG interpretation. AI-powered solutions like PMcardio help to bring more standardisation into electrocardiography and change how healthcare professionals process ECGs.
To learn more from Robert or Anthony, follow them on Twitter:
- Robert Herman, M.D. (@RobertHermanMD)
- Anthony H. Kashou, M.D. (@anthonykashoumd)
Connect with Mayo Clinic’s Cardiovascular Continuing Medical Education online at https://cveducation.mayo.edu or on Twitter @MayoClinicCV and @MayoCVservices.