Heart failure is a serious issue that has a profound impact on millions of people around the world. In the US alone, it is estimated that nearly 6.5 million people over the age of 20 live with heart failure. Heart failure is also a major killer. Some reports suggest it could account for up to 36% of all cardiovascular-related deaths. [1]
As a progressive disease, symptoms of heart failure get often overlooked, often until it’s too late. When acute heart failure occurs, every minute counts. Diagnosing the patient accurately, managing them correctly, and transferring them to an appropriate care facility can often be the deciding factor between living and dying.
We have recently talked to one of the PMcardio users, who’s a physician-scientist trainee working at a congestive heart failure outpatient clinic. To protect his privacy, we will be calling him John Smith.
John’s clinic runs a surveillance programme for patients without insurance who have previously been hospitalised with heart failure. He has recently told us an inspiring story of a patient with acute heart failure who he and his team helped save not long ago.
Here’s a short case study on how PMcardio helped John and his team to manage this patient more efficiently, speed up the decision-making process on further treatment, and eventually save this patient’s life.
Racing against time
A few weeks ago, John and his team were presented with a patient in the outpatient clinic, a 45-year-old woman, after she passed out multiple times at home and didn’t feel well. In John’s words: “When she came to us, she could barely stand and wasn’t really able to communicate. We had a limited understanding of what medicine she was taking if any, so we had to function like a triage while the emergency medical services were called.”
As it turned out, she had very low blood pressure, and her pulse was very low. When John and the team did the EKG, they immediately saw that the reason was that her heart was dangerously close to a life-threatening arrhythmia, with over 80% of her beats being PVCs (premature ventricular contractions).
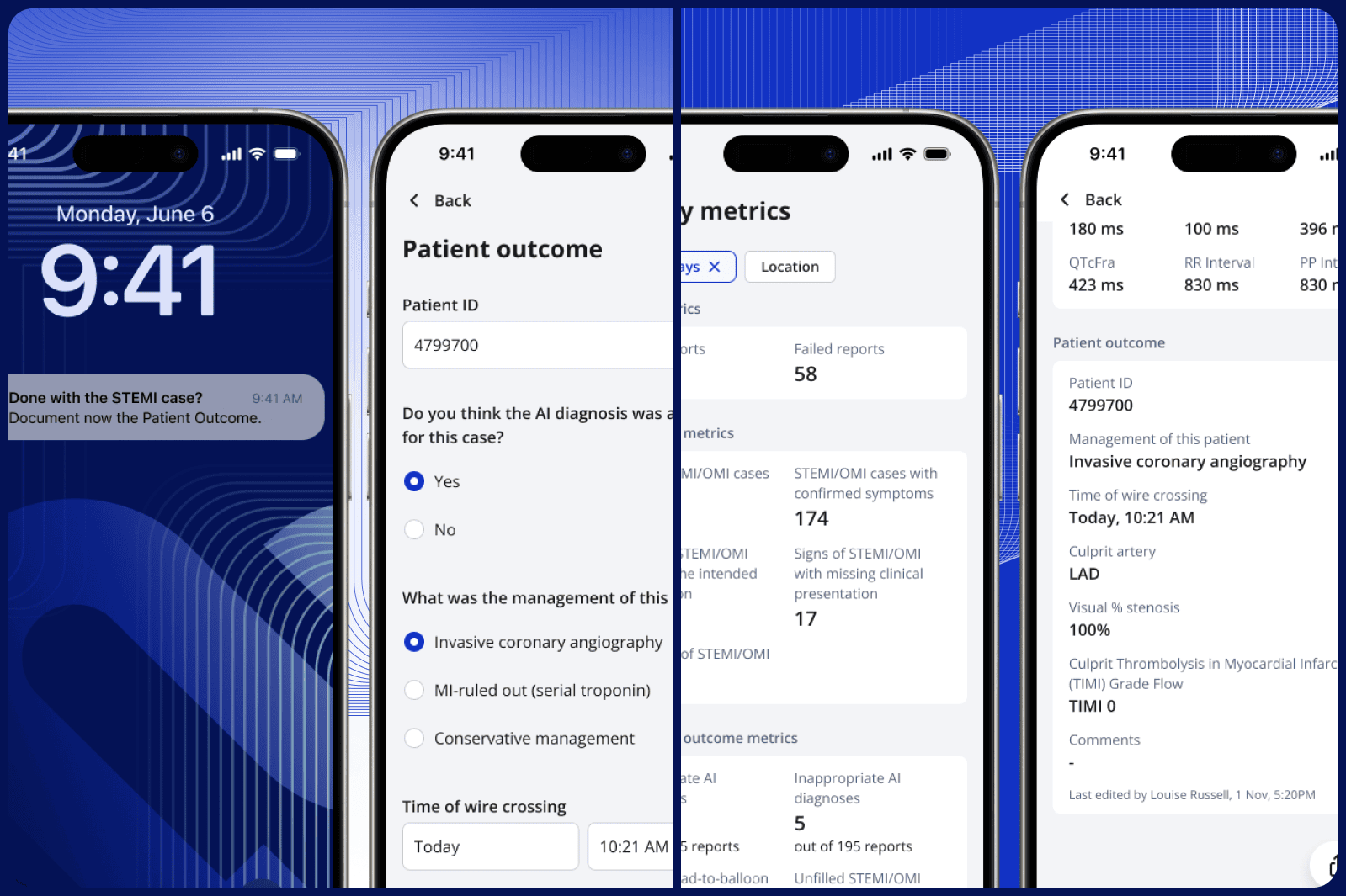
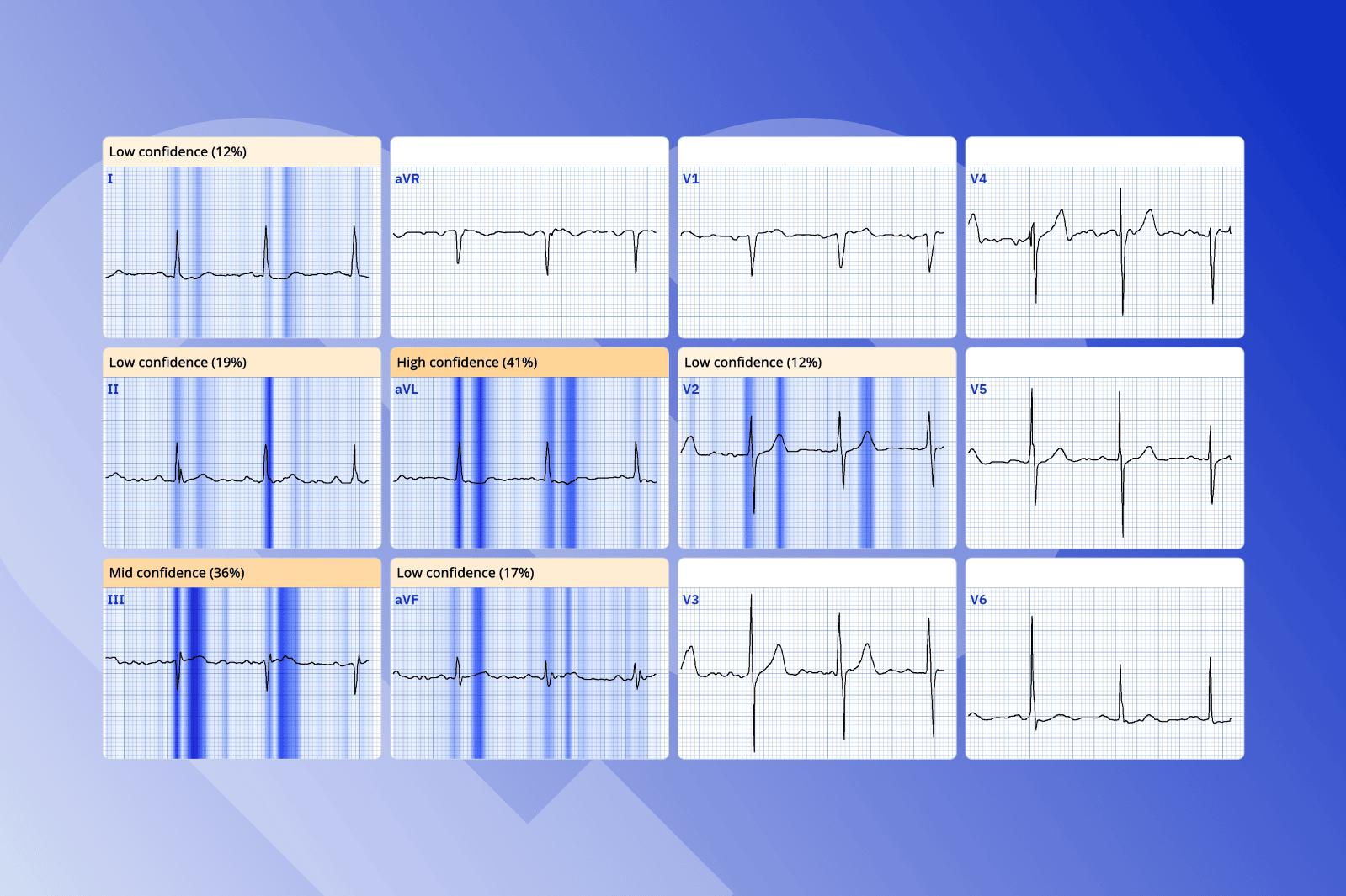
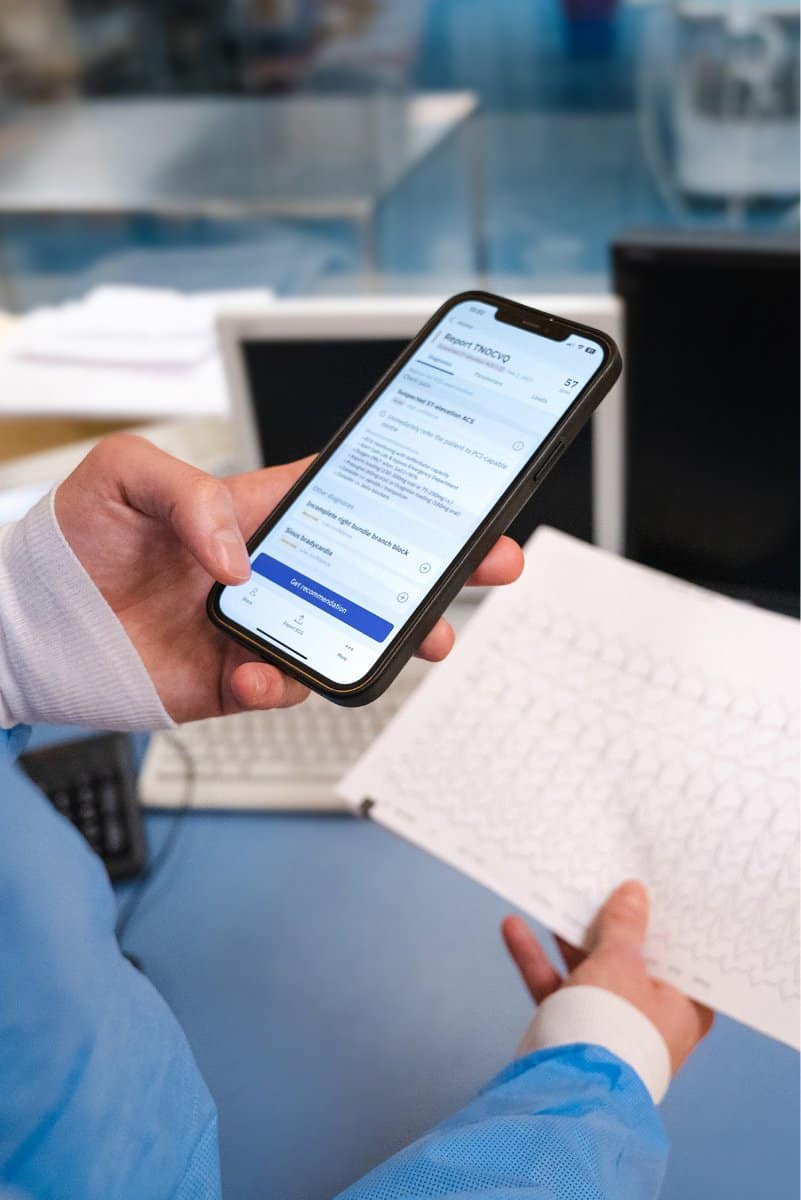
“We don’t have a cardiologist on site, so we performed an EKG in real-time with PMcardio to confirm what we thought we were seeing. The patient was very sick and needed to go to the ER. But we needed to have a plan to be able to urgently resuscitate”, continues John.
“While we could quickly identify the heavy PVC burden, PMcardio helped us see something more underneath – a dangerous prolongation of the QT interval and some other characteristics that may have been associated with digoxin toxicity. All this combined would potentially be life-threatening.
This framed our thinking around what we need to do and what we need to do very quickly – or this patient may not live. The PMcardio treatment recommendations said we needed to check for electrolyte abnormalities and that we needed to check for QT-prolonging drugs. It turns out she had both. PMcardio was spot-on.”
A positive outcome for the patient
PMcardio has proved invaluable for John in this particular case for two reasons.
One, it gave him and his team a better and clearer picture of the root cause of the patient’s problems.
As John said: “I think one of the difficulties of being a human is that we’re great at recognising patterns. But we’re bad at following through once we’ve recognised the first most obvious. So, PMcardio was our “set of unbiased eyes”. As soon as we saw how many PVCs there were, the brain shut off, and we focused on the fact that the patient needs to be taken to the ER. But when we saw prolonged QT on the PMcardio report, we took immediate action.”
Two, PMcardio has helped speed up the whole process of getting the patient the help she needed.
In John’s words: “This patient had an extremely advanced heart failure, she did not have a lot of quality tissue remaining, and of course, under this kind of strain, she was starting to develop ischemia. Ultimately – very probably – we were able to save some heart tissue because, with the help of PMcardio, we were able to let the ER know the likely cause of her presentation before she arrived. This significantly sped up the whole process.”
John and his team responded quickly and, with the help of PMcardio, could diagnose the patient accurately and provide her with proper initial care before she was brought to the emergency room. Thankfully, the outcome for the patient was positive, and she is now on the road to recovery.
Stay on the pulse with our newsletter
Your submission was successful
Artificial intelligence – a doctor’s second pair of eyes
Physicians in primary or emergency care perform many EKGs and deal with cardiac patients, often with no cardiologist to consult. They either use remote consultations or refer the patient further to secondary care. As John said: “We do have licenced physicians on-site, but they’re not cardiologists; they’re typically early out of their training; they may be residents that are being supervised remotely. And so there’s not necessarily a lot of confidence, even if there is expertise.”
Often, they would need a second opinion to confirm what they already thought or bring another perspective into a patient’s case. Artificial intelligence brings this kind of expertise into primary care. John aptly called it – an “expertise extender”.
An AI-powered tool like PMcardio provides that extra pair of eyes that helps physicians and medical professionals be more confident and quicker in their clinical decisions.
“PMcardio helped us make sure we’re on the right track. Or to give us a better picture of what to expect from the patient. We snap a picture of an EKG and get a pretty good sense of what we are dealing with. PMcardio makes me look at things much more holistically,” concludes John.