We are thrilled to announce the launch of the AI-ECG TIMI Study, a novel, international, multi-center observational study aimed at validating the use of AI to improve the detection and management of acute coronary syndromes (ACS).
This study, running from December 2024 to December 2025, represents a crucial step in understanding the pathophysiological changes in ACS patients with plaque rupture and understanding their impact on 12-lead ECG patterns.
Current Gaps in Evidence
Despite significant advancements in the understanding of acute coronary syndromes due to plaque rupture and thrombotic occlusions, the AI-ECG TIMI study will seek to address several key gaps in evidence:
- Lack of Standardized ECG Data at Critical Moments: To date, no study has collected standard 12-lead ECGs (continuously) recorded precisely at the time of invasive coronary angiography. This critical gap limits our ability to fully understand the relationship between STEMI equivalent ECG patterns and culprit coronary vessel status during acute coronary events.
- Objective Quantitative Assessment of Microvascular Perfusion in Culprit Vessels: There is currently no objective method for the accurate assessment of microvascular perfusion in territories supplied by culprit vessels. Thus we do not know whether the occlusion is causing an irreversible infarction, or open coronary arteries truly have good microvascular perfusion.
- Dynamic Nature of Acute Coronary Syndromes : Thrombotic occlusion due to plaque rupture is dynamic—up to one-third of STEMI culprit lesions may spontaneously re-open (reperfuse), a phenomenon that can manifest on ECGs but remains difficult to predict and manage effectively. The 12-lead ECG recorded at patient admission may not be reflective of culprit coronary vessel status at angiography (visible hours later).
- Untapped Potential of AI-Based ECG Interpretation: While AI has shown promise in improved ECG interpretation, there remains significant untapped potential in its ability to distinguish between actively occluded and recanalized culprit coronary vessels in acute myocardial infarction patients.
- Potential of ECG as a Non-invasive Marker of Reperfusion Success: Up to 50% of STEMI patients with patent (TIMI-3 flow) vessels after intervention have microvascular obstruction and a poor long-term prognosis despite treatment. Historically ECG has been used as a marker to detect treatment success upon administering thrombolysis (based on resolution of the ST segment). The AI-ECG TIMI study will build on this potential.
- Lack of Real-World Validation: AI-assisted chest pain patient triage in emergency departments lacks robust validation of its real-world use, highlighting the need for studies like AI-ECG TIMI to demonstrate its clinical efficacy in everyday settings.
Study Overview: A Global Effort to Enhance Cardiac Diagnostics
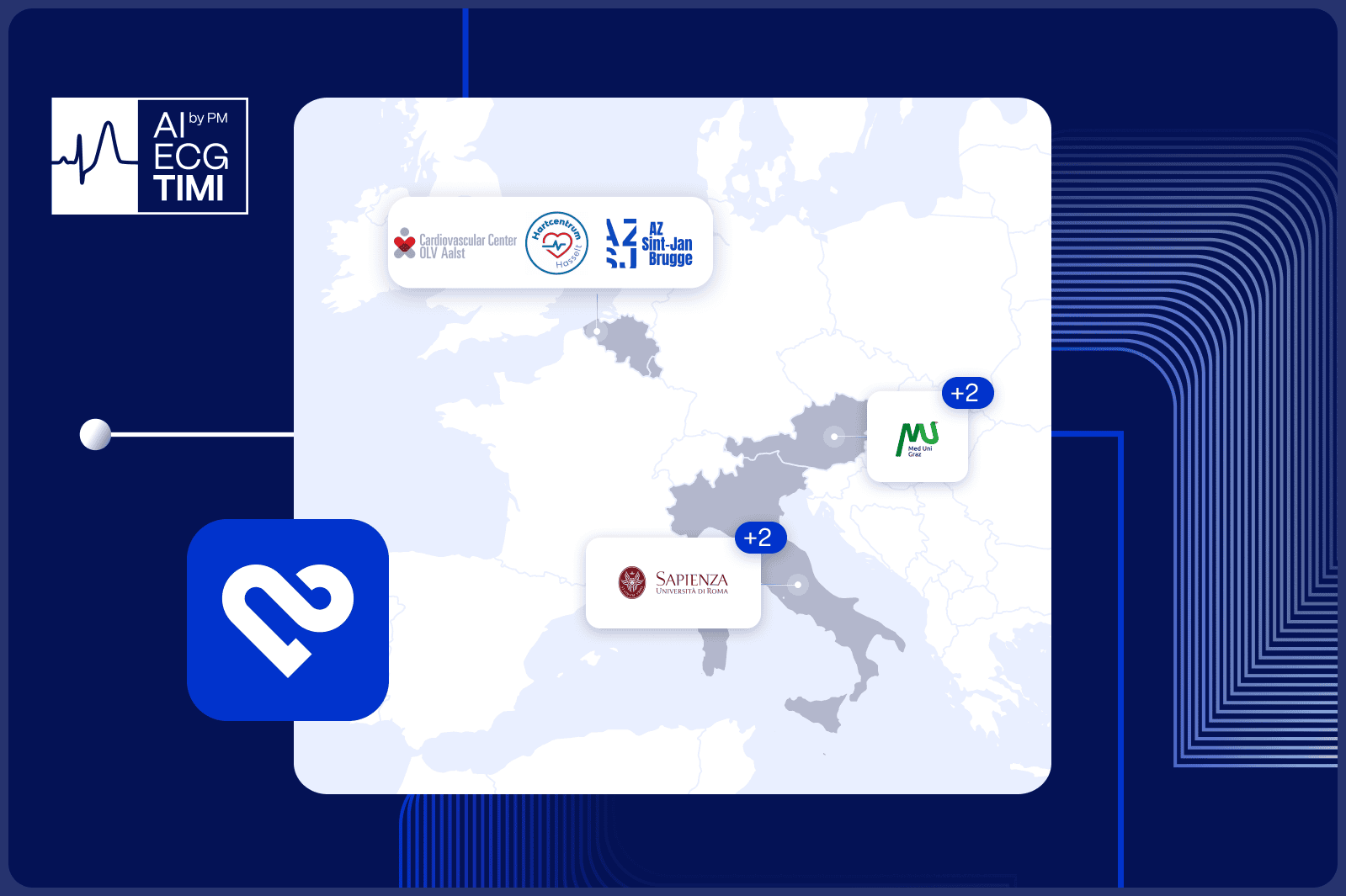
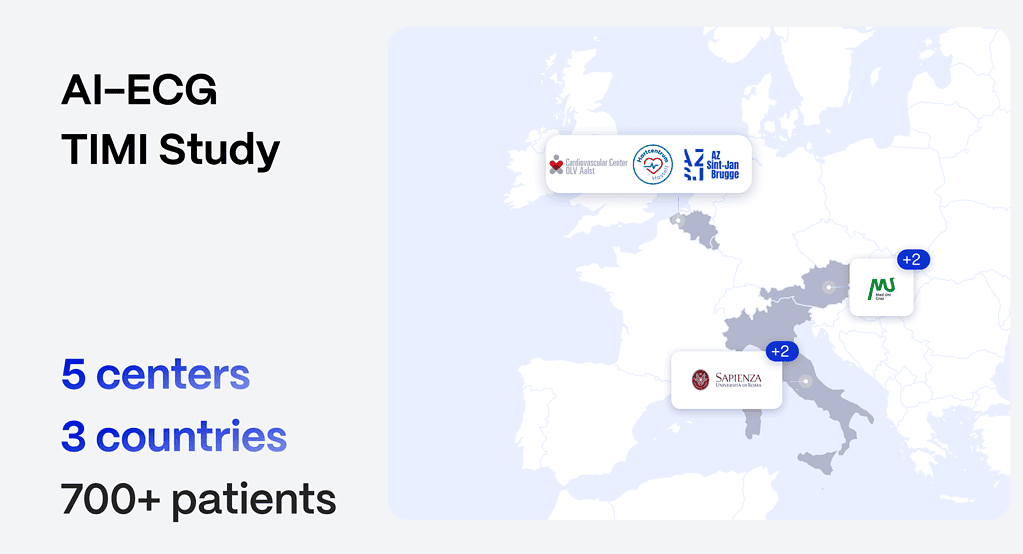
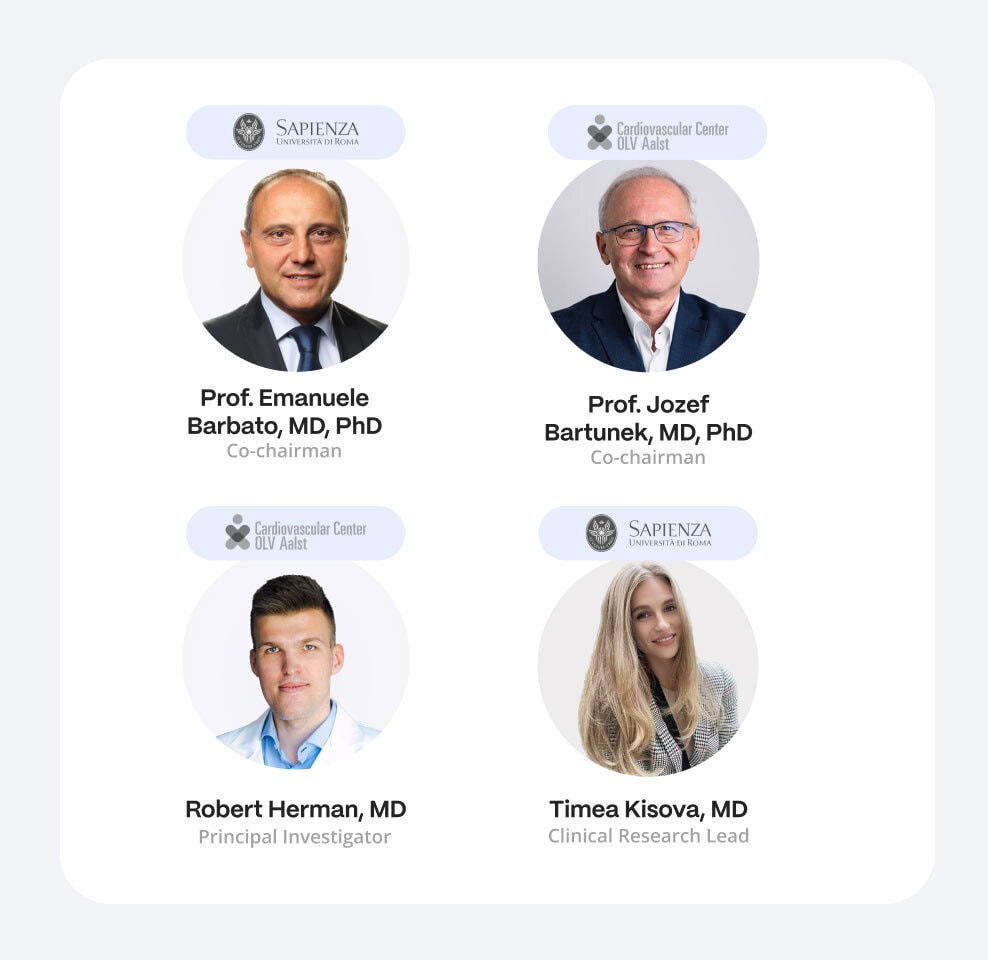
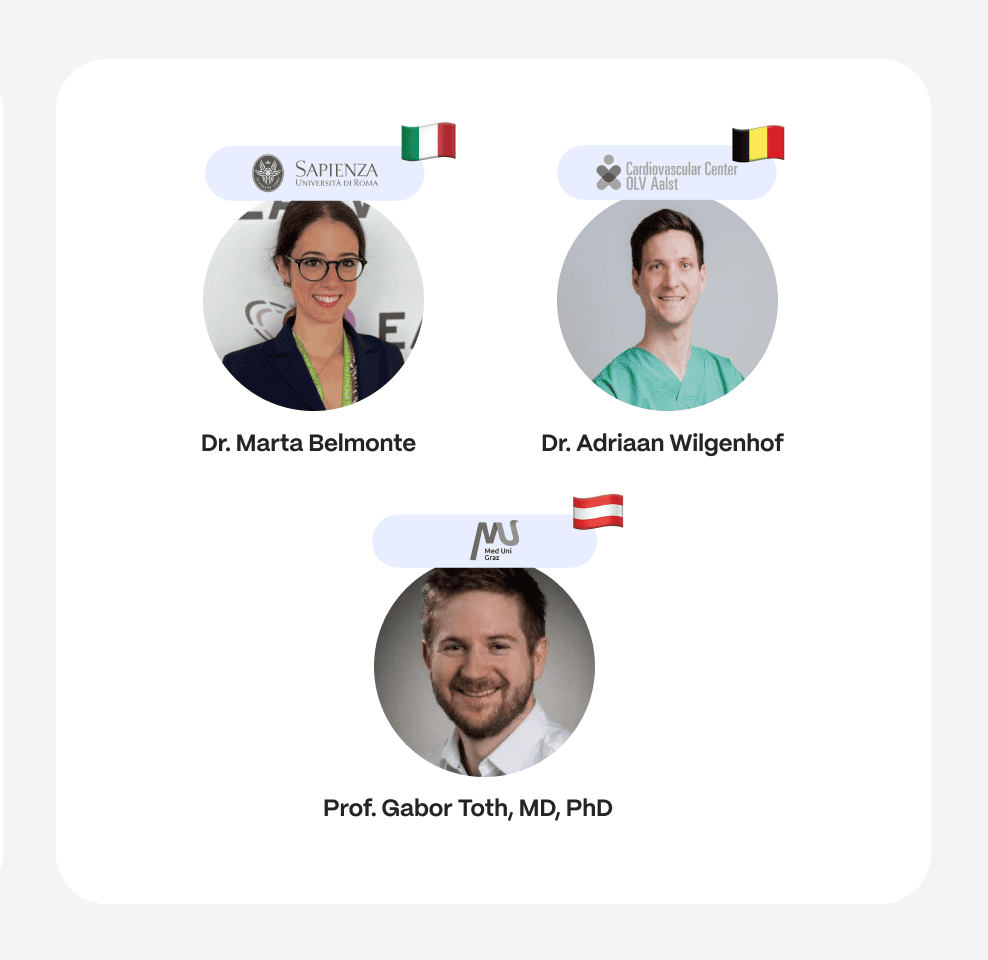
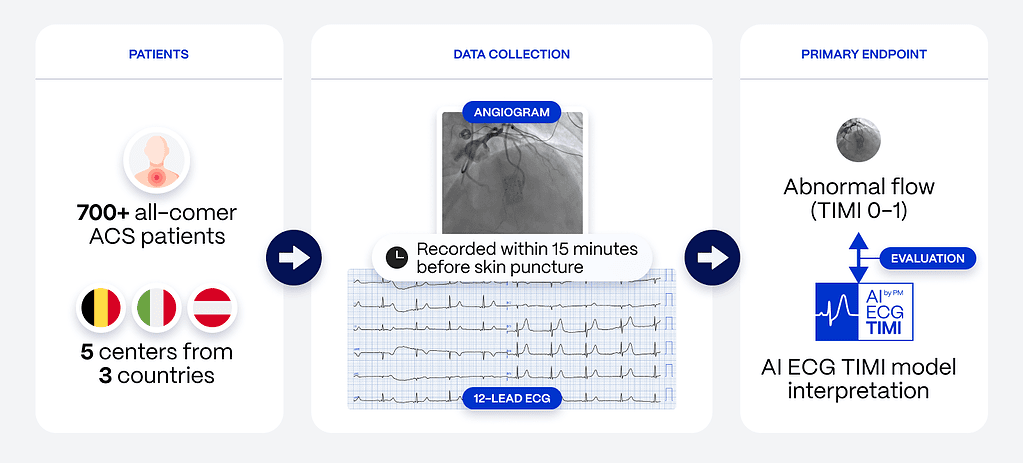
The AI-ECG TIMI Study (ClinicalTrials.gov Identifier: NCT06528821) will enroll over 700 patients across three countries and five centers, all presenting with acute coronary syndromes. By leveraging AI-driven ECG interpretation, the study aims to predict coronary blood flow alterations, specifically occlusive myocardial infarction, a condition requiring rapid diagnosis and intervention.
This multi-center approach ensures that the AI model is validated across diverse patient populations and clinical settings, providing robust data that will improve the model’s applicability across healthcare systems (ctv.veeva.com).
The full design and rationale of the AI-ECG TIMI Study are published in JSCAI (https://www.jscai.org/article/S2772-9303(24)02183-5/fulltext) and in JSCAI Special Issue March 2025 “The Role of Artificial Intelligence in Cardiovascular Interventions”.

Primary Outcome Measure: Diagnostic Accuracy of the AI-ECG TIMI Model
The primary goal of the AI-ECG TIMI Study is to assess the diagnostic accuracy of the AI model in identifying patients with actively occluded coronary arteries (TIMI flow grade 0-1) at the time of invasive coronary angiography.
Using a single-standard 12-lead ECG, the AI model will be evaluated on its accuracy, sensitivity, specificity, positive and negative predictive values, and F1 scores over the course of one year. This validation process is essential for establishing the model’s capability to enhance real-time clinical decision-making in acute care settings.
Secondary Outcome Measures: Expanding the Scope of AI Performance
In addition to the primary outcome, the study will explore several secondary measures that further analyze the model’s performance:
- Subgroup performance: The AI-ECG TIMI model’s accuracy will be evaluated across different subgroups, including demographics, risk factors, co-morbidities, electrocardiographic profiles, and culprit artery territories.
- Correlating OMI definitions with myocardial perfusion: The study will correlate established OMI definitions using routine angiographic and laboratory parameters with myocardial perfusion status, as measured by correlation coefficients, to refine the model’s diagnostic capabilities.
- ECG prediction of mechanical reperfusion: The model’s raw numeric predictions (on a scale of 0 to 1) will be correlated with myocardial perfusion grading post-percutaneous coronary intervention (PCI), helping to evaluate the AI’s predictive power regarding treatment success.
- Expert ECG interpretation: A blinded assessment of expert ECG interpretations will be conducted to compare the accuracy, sensitivity, specificity, and predictive values of human interpretation with the AI model’s performance. The study will also examine inter-rater variability among experts.
- STEMI equivalent ECG patterns: Researchers will assess the prevalence of STEMI-equivalent ECG patterns and their correlation to TIMI flow grade at angiography, providing insights into non-traditional indicators of occlusion.
- STEMI equivalent patient subgroup analysis: The study will analyze patients with STEMI equivalents who are stratified based on timing of invasive management (immediate vs. standard of care), examining peak troponin levels, left ventricular ejection fraction (LVEF) at discharge, and length of hospital and intensive care unit (ICU) stays. Life-threatening arrhythmias and TIMI scores will also be tracked.
Advancing Global Cardiovascular Care
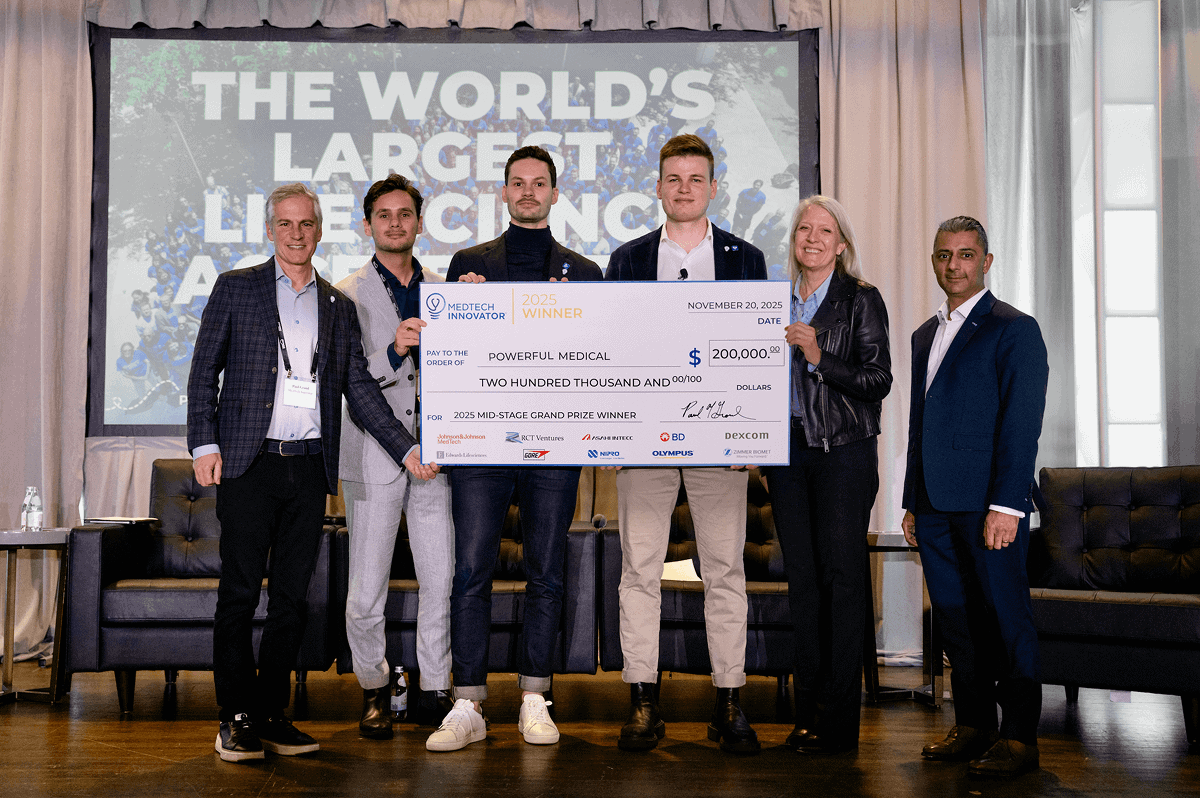
At Powerful Medical, we are committed to drastically reducing deaths from occlusion myocardial infarction. The AI-ECG TIMI study represents a bold step forward in refining our AI technology for earlier and more accurate detection, equipping clinicians with the tools to intervene swiftly and effectively.
Our goal is to transform cardiac diagnostics, not only by enhancing clinical workflows and improving patient outcomes but also by augmenting the chest pain patient journey – delivering faster, more precise diagnoses and making a significant impact on reducing MI-related mortality.