Accurate interpretation of 12-lead electrocardiograms (ECGs) is crucial in the timely management of acute coronary syndromes (ACS). Inconsistent recognition of subtle yet significant ECG patterns can lead to delays in treatment or unnecessary interventions1. This is particularly challenging in acute myocardial patients with spontaneous recanalization of the culprit artery or post-treatment (mechanical reperfusion) changes2.
Ensuring timely and precise differentiation between active occlusion and reperfusion is essential for optimizing patient outcomes and resource allocation3. Patients who previously had active ischemia due to acute coronary occlusion, but now exhibit reperfusion and resolution of symptoms, may have less urgency for coronary intervention, although this remains dependent on clinical context and ongoing assessment..
By leveraging advanced AI technology, PMcardio addresses these diagnostic complexities, providing clinicians with actionable insights and enhancing decision-making in real time5.
Given its fast acquisition, the 12-lead ECG remains a cornerstone in the early detection of thrombotic acute coronary occlusion due to plaque erosion or rupture6. However, in approximately 30% of STEMI patients, spontaneous recanalization (TIMI-3 flow) occurs prior to coronary angiography.
Guidelines regarding the optimal timing for PCI in these patients with unstable lesions and partially restored blood flow remain unclear, particularly when this coincides with the resolution of chest pain. Thus differentiating these two states of the culprit coronary artery is essential for accurate diagnosis, optimal management and resource utilization.
To address these complexities, we have refined our AI-based ECG interpretation tool to provide more granularity in ECG analysis of acute myocardial infarction. By integrating the newest version of the STEMI AI ECG Model within an innovative Acute Coronary Syndrome (ACS) Pathway, PMcardio empowers healthcare providers to tailor management strategies for these patients with precision and efficiency.
Three Key Output States of the PMcardio Module
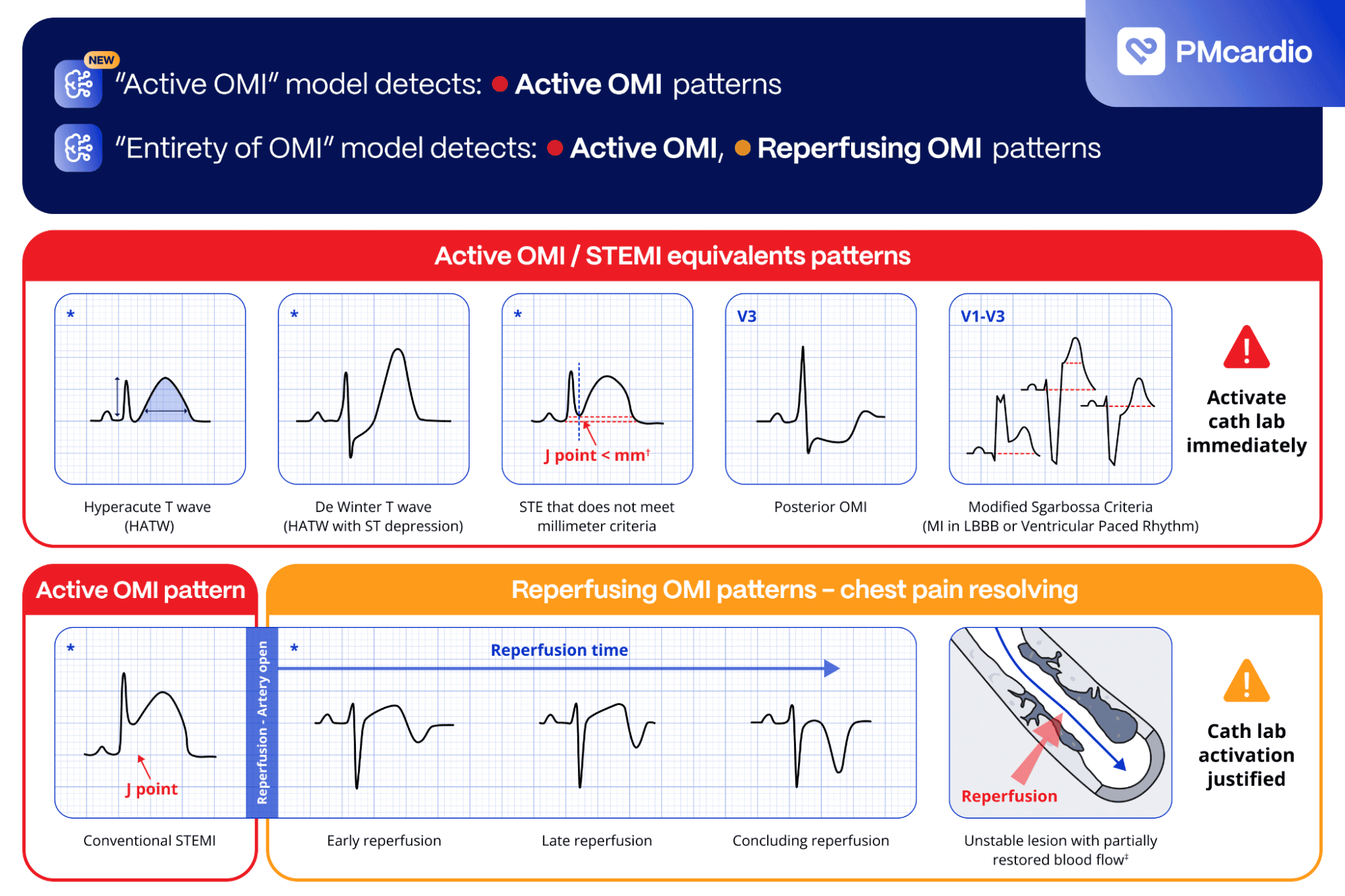
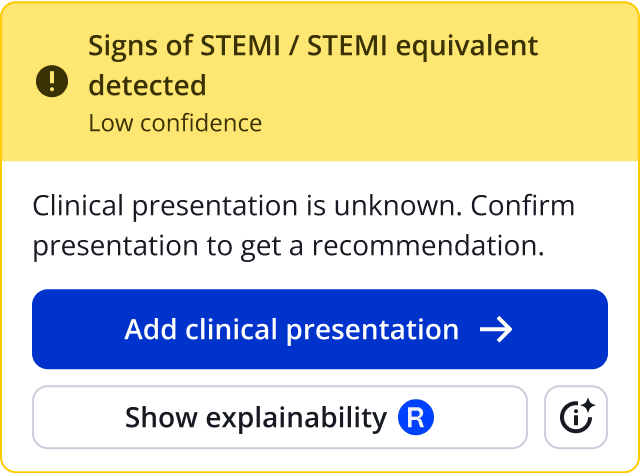
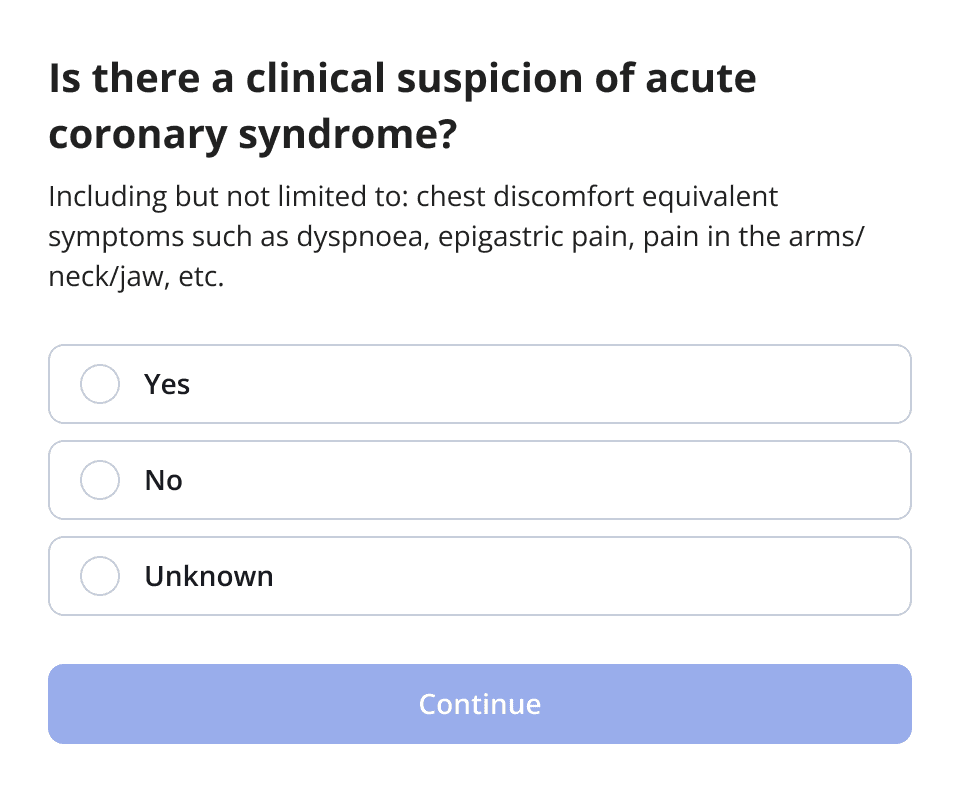
The PMcardio ACS Module categorizes ECG findings into three actionable states:
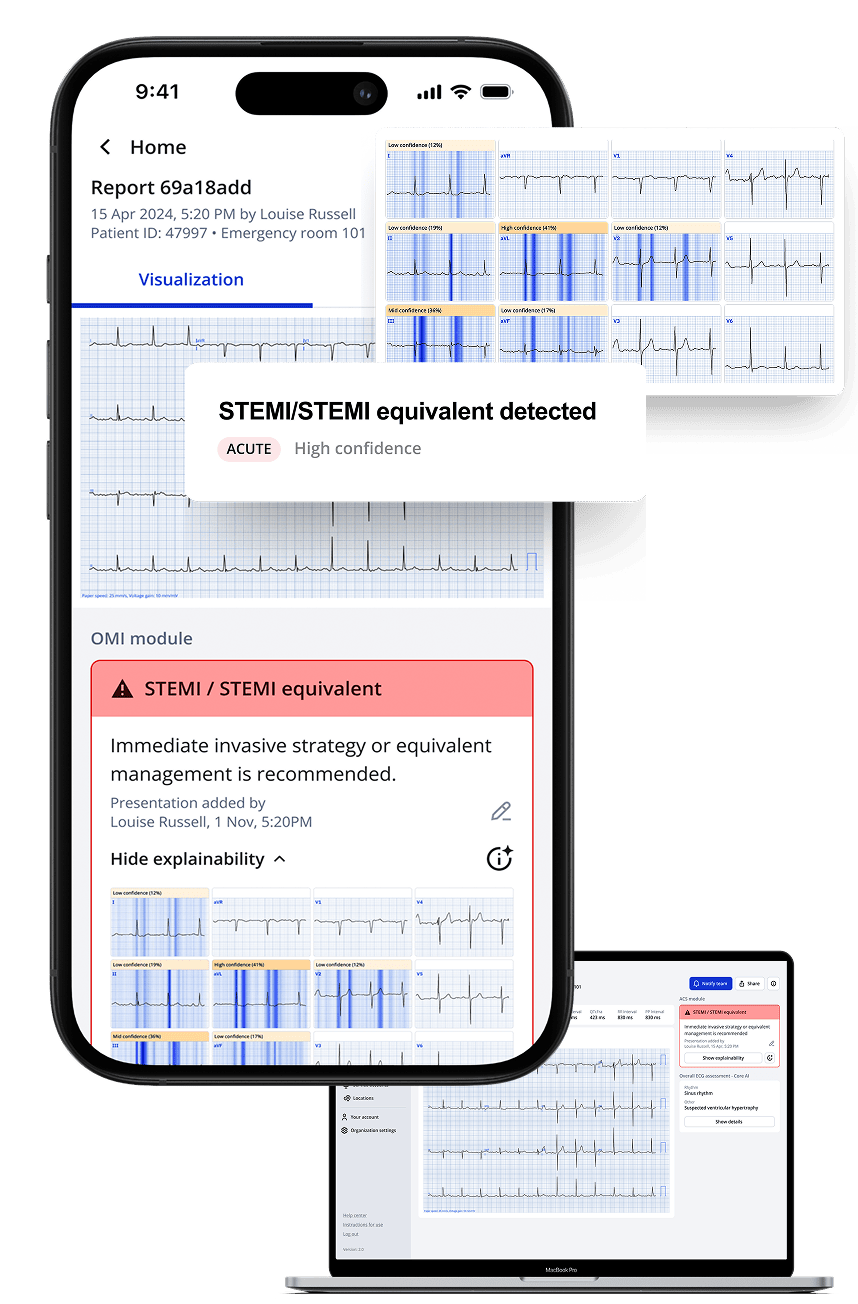
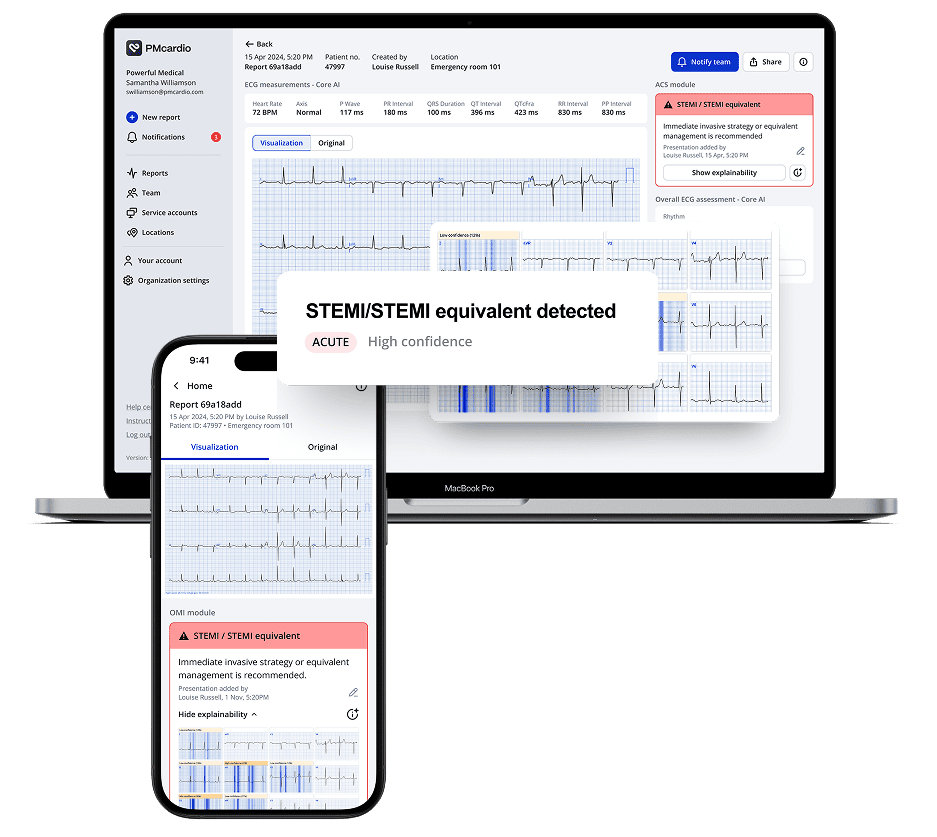
1. STEMI / STEMI Equivalent
Also called “Active OMI”, this state indicates active coronary occlusion at the time of the ECG recording. The AI model identified STEMI meeting formal millimeter criteria and STEMI-equivalent patterns suggestive of ongoing arterial blockage, such as hyperacute T-waves (HATW), De Winter T-waves, posterior STEMI patterns, and Modified Sgarbossa Criteria in LBBB or ventricular paced rhythms.
Immediate invasive strategies, such as primary PCI, are recommended in line with current clinical guidelines. In accordance with the European Society of Cardiology (ESC) guidelines, primary PCI should be performed promptly in patients with ST-segment elevation myocardial infarction, ideally within 90 minutes, and 120 minutes of first medical contact if non-PCI center is involved.7
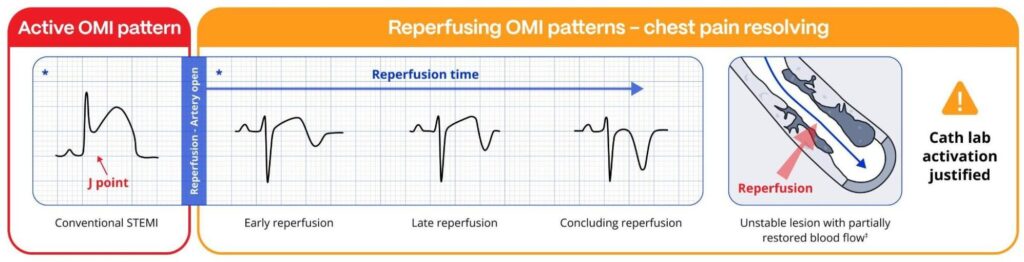
2. Reperfused OMI
This output state reflects an artery that was recently acutely occluded (STEMI / STEMI equivalent) but has since reopened. Clinical presentations often align with resolution of chest discomfort or its equivalent. The model’s ability to detect reperfusion patterns enables clinicians to differentiate between active occlusion and reperfusion states, better informing the clinician of the optimal timing for interventions.
Wellens syndrome is a classic example of an anterior reperfusion pattern, characterized by biphasic or deeply inverted T-waves in the precordial leads (typically V2-V3)8. These findings may indicate spontaneous reperfusion but carry a high risk of re-occlusion if left untreated. PMcardio’s AI can differentiate between the currently reperfused state and active blockage, enabling clinicians to act decisively based on the specific clinical context.
3. No signs of Occlusive Myocardial Infarction
While no active OMI or STEMI equivalent is detected, the absence of findings does not rule out myocardial infarction. Patients should undergo further evaluation, including serial ECG and troponin testing, to confirm or exclude acute myocardial infarction if suspicion of ACS is present.
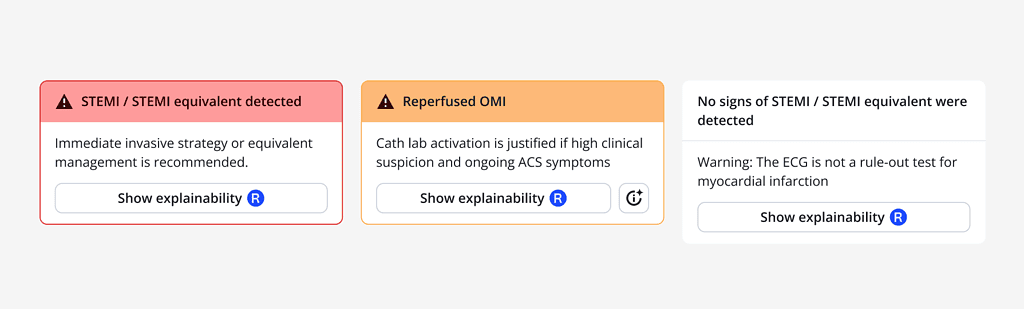
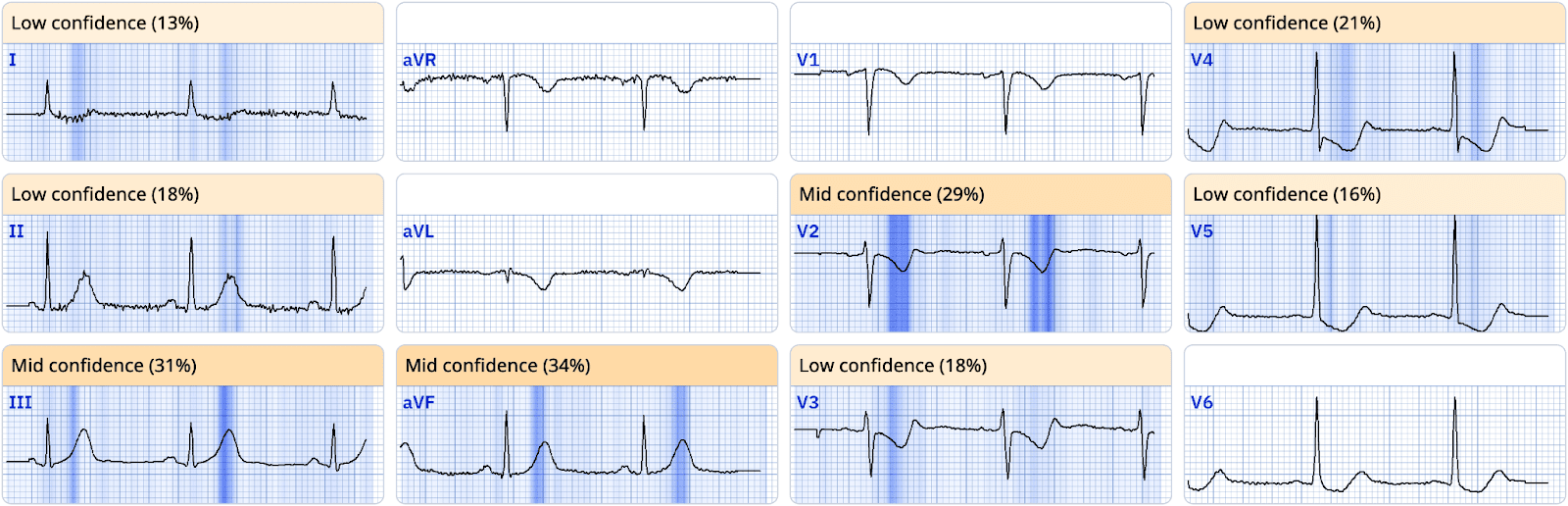
Enhancing Clinical Decision-Making with Explainability and Customization
The PMcardio platform provides explainability for each positive AI-generated output, ensuring that clinicians can understand the rationale behind the model’s predictions. Additionally, the ACS Pathway allows institutions to customize management protocols, aligning with their unique workflows and clinical guidelines.
The Role of Reperfusion Patterns in Diagnosis and Management
Reperfusion patterns on the ECG, such as terminal T-wave inversions seen in Wellens syndrome, provide critical clues to the patient’s clinical trajectory. These patterns often emerge during pain-free intervals and can indicate either spontaneous or intervention-related reperfusion8. Recognizing these patterns and distinguishing them from active occlusion is crucial for preventing unnecessary interventions while ensuring timely care for patients at risk of re-occlusion.
By distinguishing between active occlusion, reperfusion, and old myocardial infarction patterns, the PMcardio platform equips healthcare providers with the tools to:
- Improve diagnostic accuracy
- Expedite time-to-treatment (E2B times)
- Avoid unnecessary cath lab activations
- Ensure effective microvascular reperfusion after intervention
Bridging the Gap in ACS Management
PMcardio’s enhanced capabilities represent a significant advancement in the management of ACS. The platform supports clinicians in delivering optimal care for patients with both classic STEMI presentations and more nuanced equivalent patterns. This innovation aligns with our commitment to improving health equity and ensuring that every patient receives timely and accurate diagnosis and treatment.
Optimize STEMI patient pathway with certified AI
The impact of PMcardio at the Cardiovascular Centre Aalst, Belgium:
- 68% reduction in false positive STEMI alerts
- 100% sensitivity in true positive STEMI patients
- 34% reduction in ECG to balloon time for STEMI patients
- 50% decrease in door-to-ECG time month-over-month
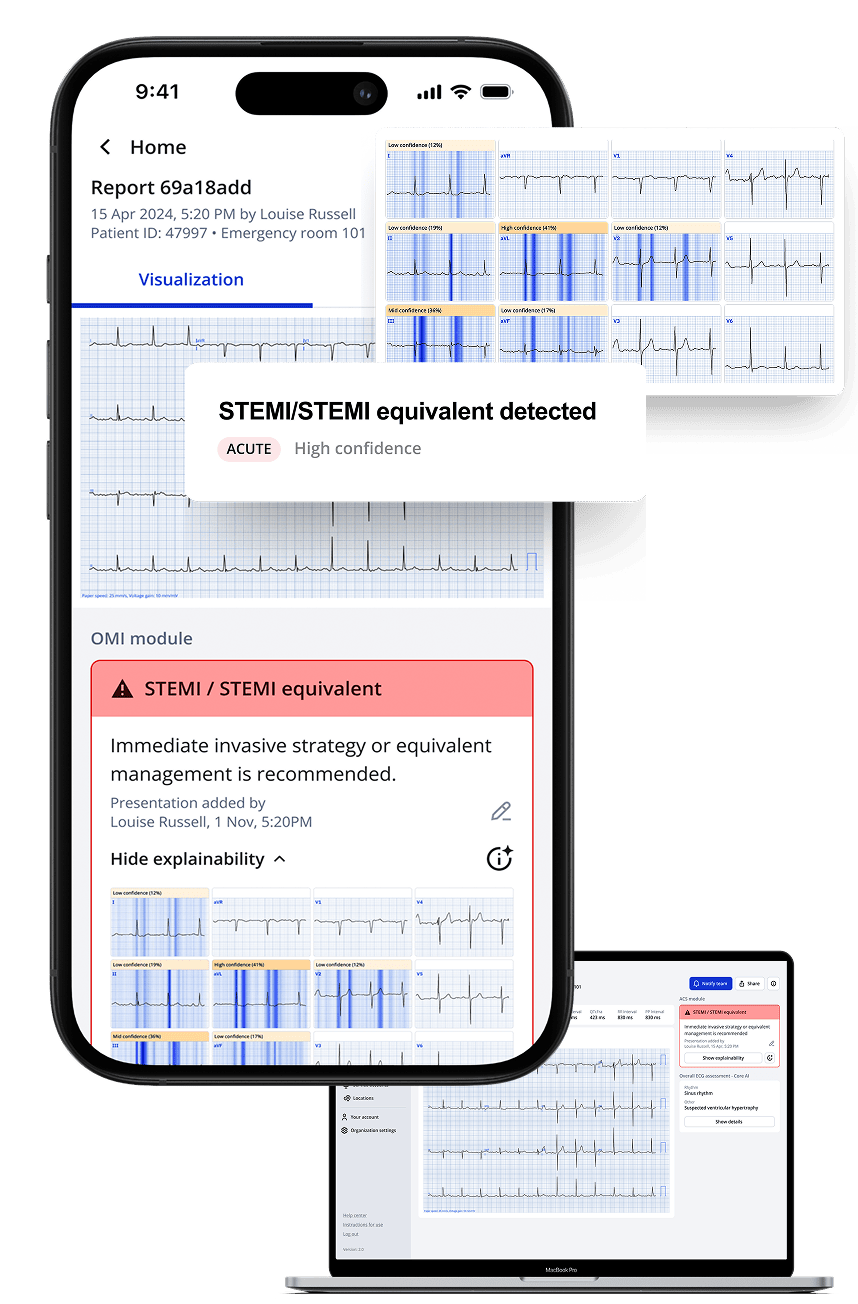
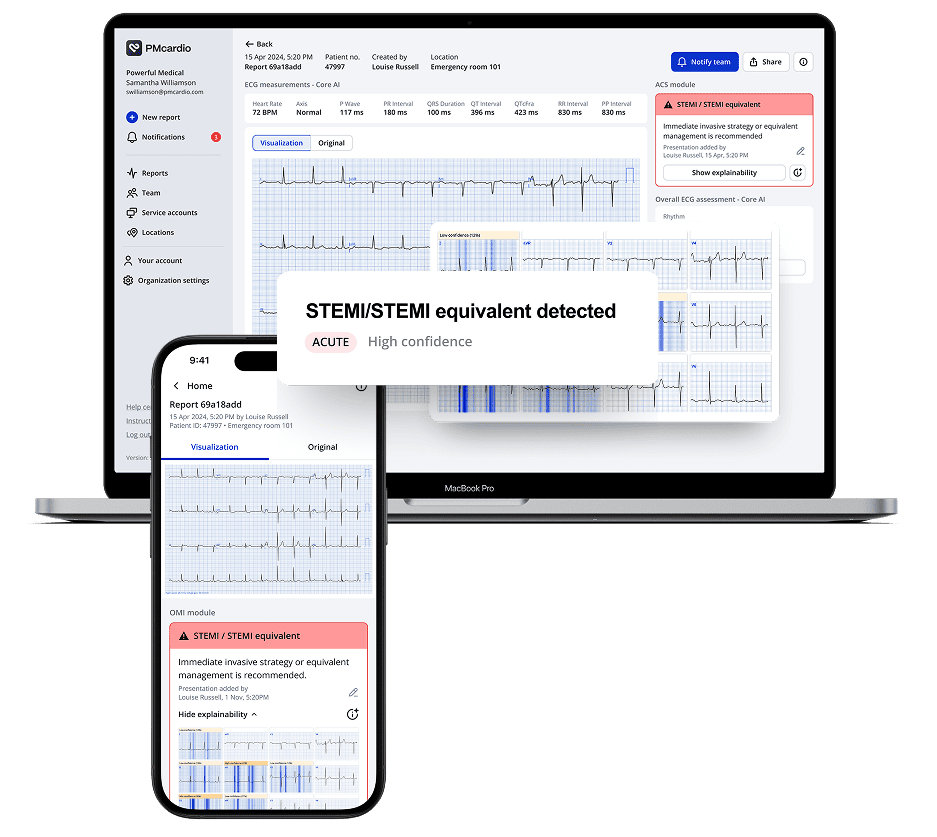
Introducing STEMI Team Notification Functionality
Timely intervention is the single most important predictor of survival in STEMI patients. According to international guidelines, patients presenting with chest pain should have their ECG interpreted for signs of STEMI within 10 minutes of first medical contact9. Furthermore, STEMI patients should be referred to a primary PCI-capable center and have their occluded artery reopened within 90 minutes to maximize survival outcomes9.
However, these critical timeframes are often not met. Studies show that only 17% of STEMI patients presenting to non-cardiac centers receive treatment within guideline-compliant windows 10. The challenges stem from delayed identification of STEMI equivalents at the first point of contact, compounded by barriers to efficient ECG transmission and streamlined team activation.
PMcardio’s STEMI Team Notification Functionality streamlines communication and accelerates care delivery through manual and automatic alerts. Manual notifications empower nurses and ED physicians to notify downstream clinicians, like interventional cardiologists, about critical cases via customizable SMS, email, or push notifications. Automatic notifications, triggered by PMcardio’s STEMI detection, eliminate human intervention, ensuring rapid alerts in high-volume ECG environments while integrating seamlessly into hospital workflows.
During on-call hours, when cardiologists may struggle to locate a patient’s ECG or make cath lab activation decisions with incomplete data, PMcardio provides immediate access to the patient’s ECG, diagnosis, and other key details. With a single click, clinicians can access the full report and take the necessary steps, whether activating the team or issuing a STEMI stop alert, ensuring swift and informed decision-making.
By closing communication gaps and optimizing team coordination, PMcardio’s STEMI notifications align care with guideline-recommended timeframes, improving survival outcomes when every minute matters. From its clinical implementation at the Cardiovascular Center Aalst, PMcardio has demonstrated its ability to reduce false-positive STEMI alerts by 67%, significantly improving accuracy and resource allocation. Furthermore, it has been shown to reduce time to PCI through faster downstream STEMI team activation by 30% for typical STEMI cases, and by over 80% in STEMI equivalents.
PMcardio’s STEMI Team Notification streamlines communication and accelerates care with manual and automatic alerts. Nurses and ED physicians can manually notify clinicians via SMS, email, or push notifications.
Automatic alerts triggered by STEMI detection ensure rapid, seamless communication, enhancing workflow efficiency in high-volume ECG settings.
Case Example: Differentiating STEMI/STEMI Equivalent and Reperfused OMI
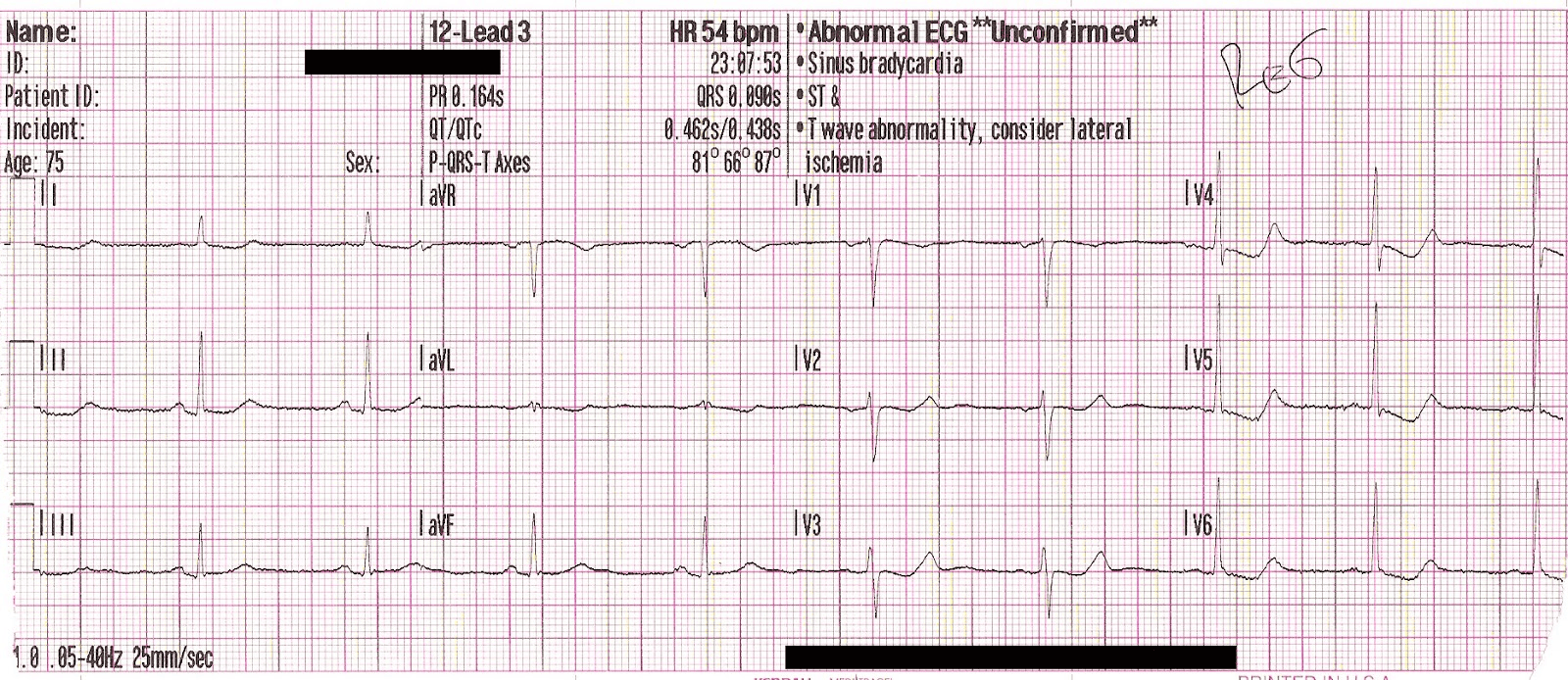
A male patient with acute chest pain and shortness of breath contacted Emergency Medical Services (EMS), and the following ECG was recorded by paramedics on scene:
ECG1:
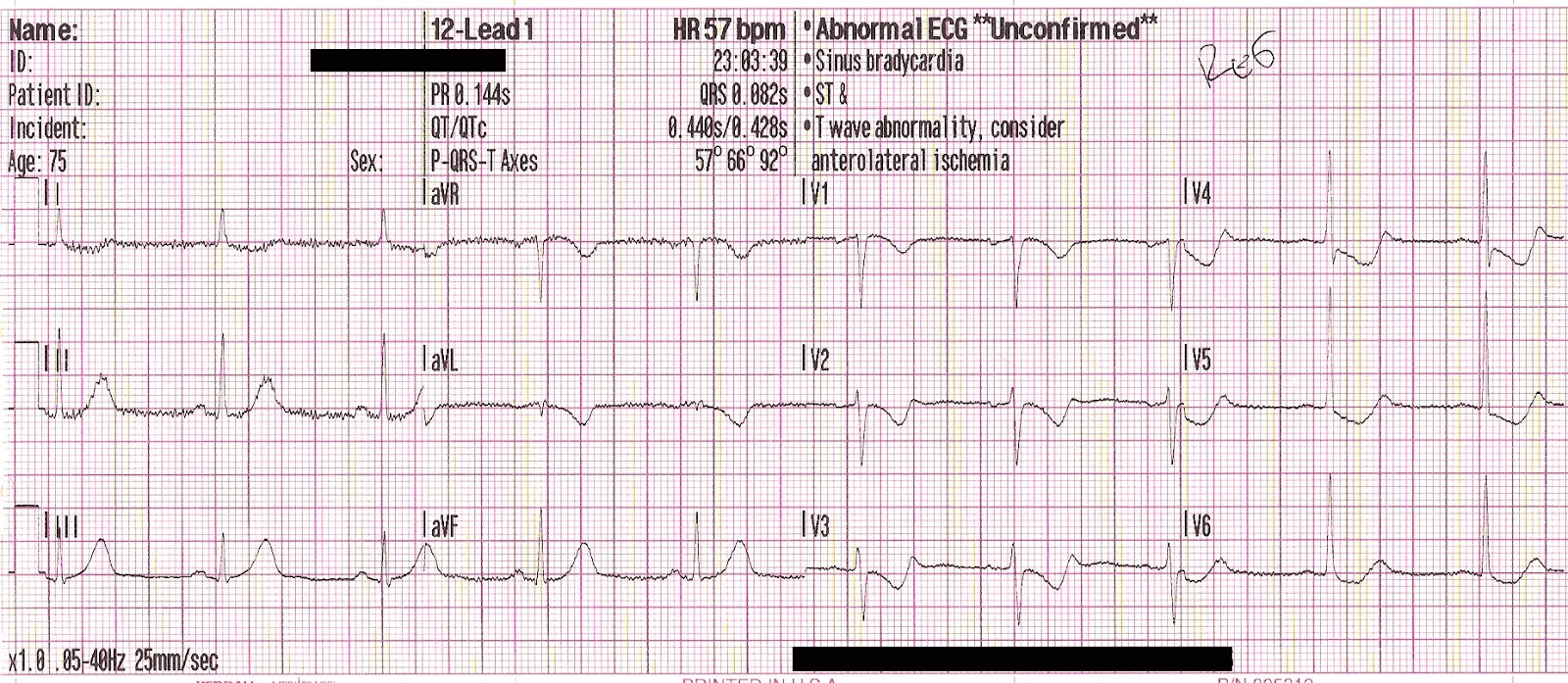
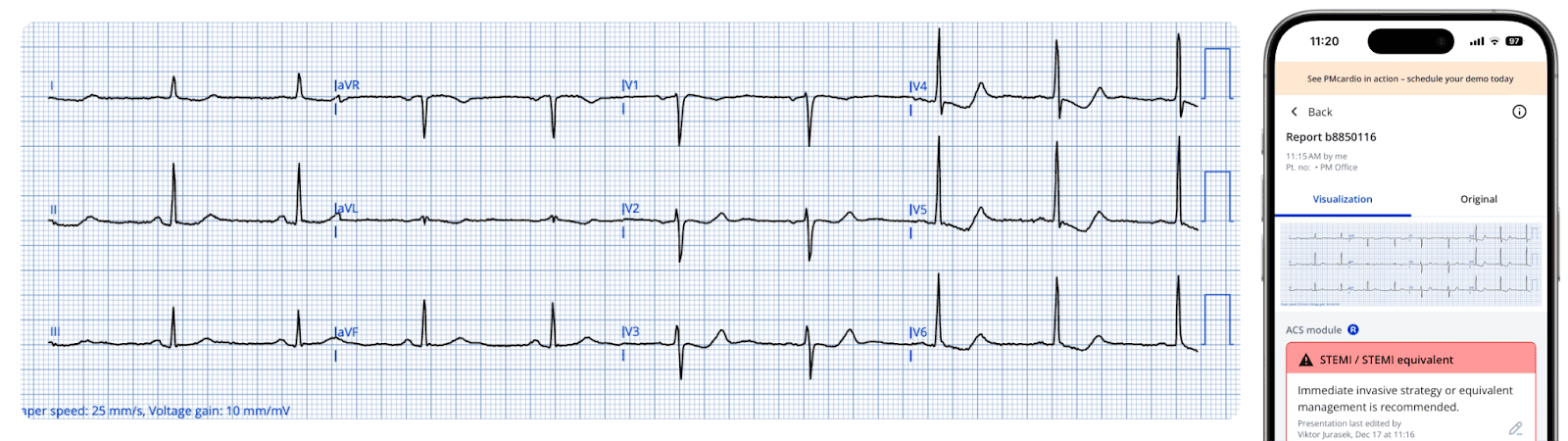
Below is the module result for this ECG, which correctly identifies STEMI/STEMI-equivalent findings consistent with active occlusion myocardial infarction.
Paramedics promptly administered aspirin and nitroglycerin, resulting in rapid resolution of the patient’s chest pain. Serial ECGs (shown below) were recorded over the next 20 minutes during transport to the PCI center, with resolving pain.
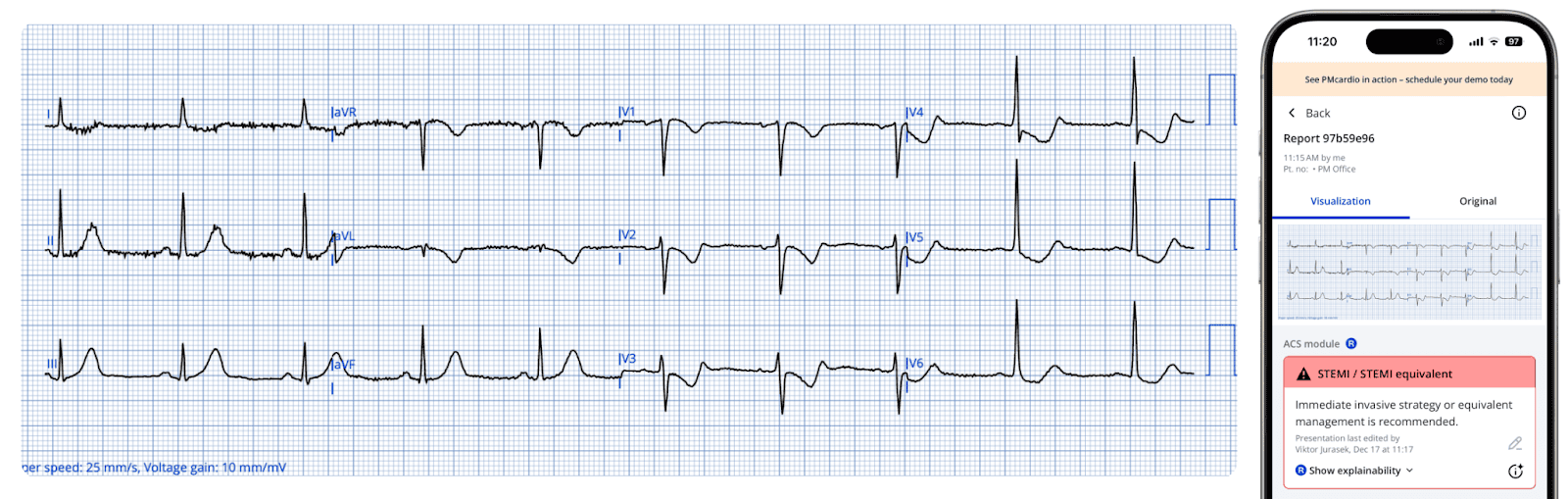
ECG2:
The inferior hyperacute T waves have resolved, and the ischemic ST depression in the precordial leads has shown some improvement.
ECG3:
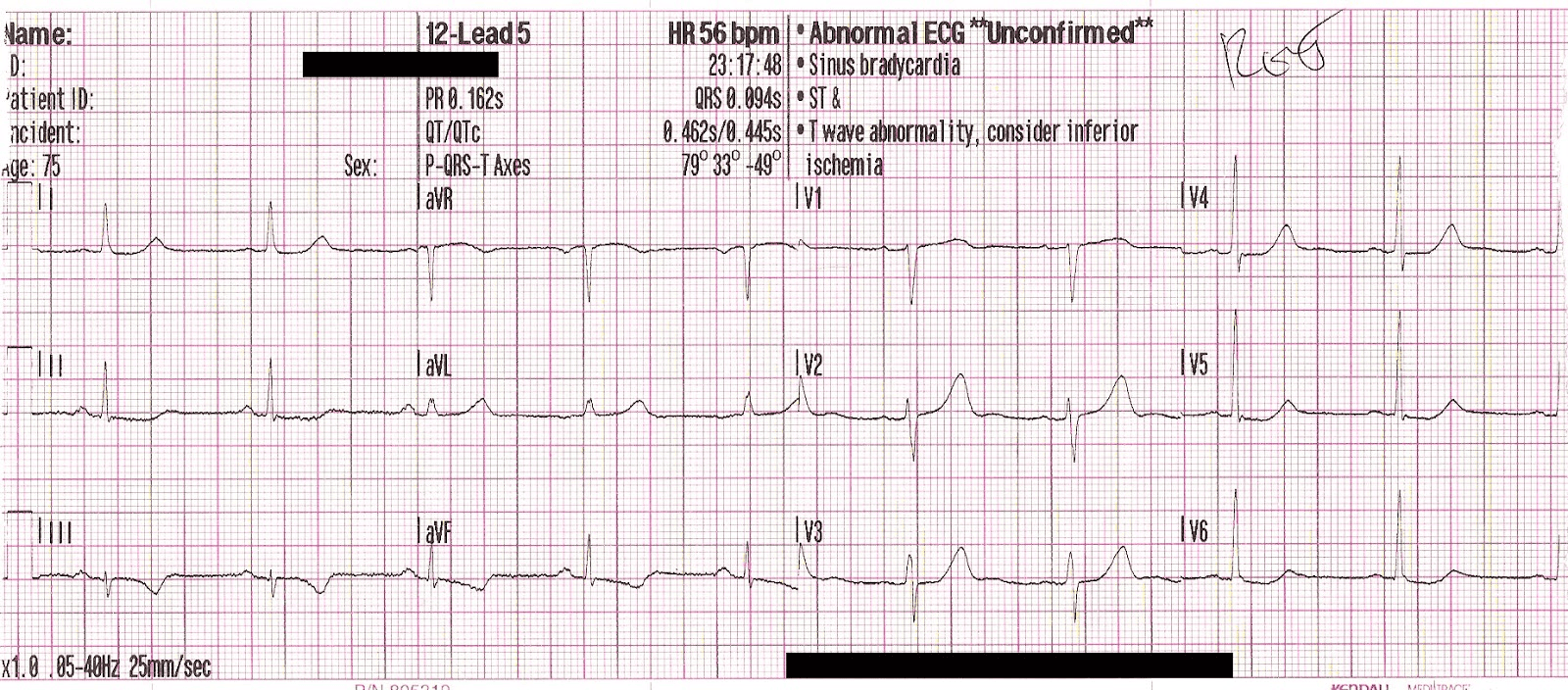
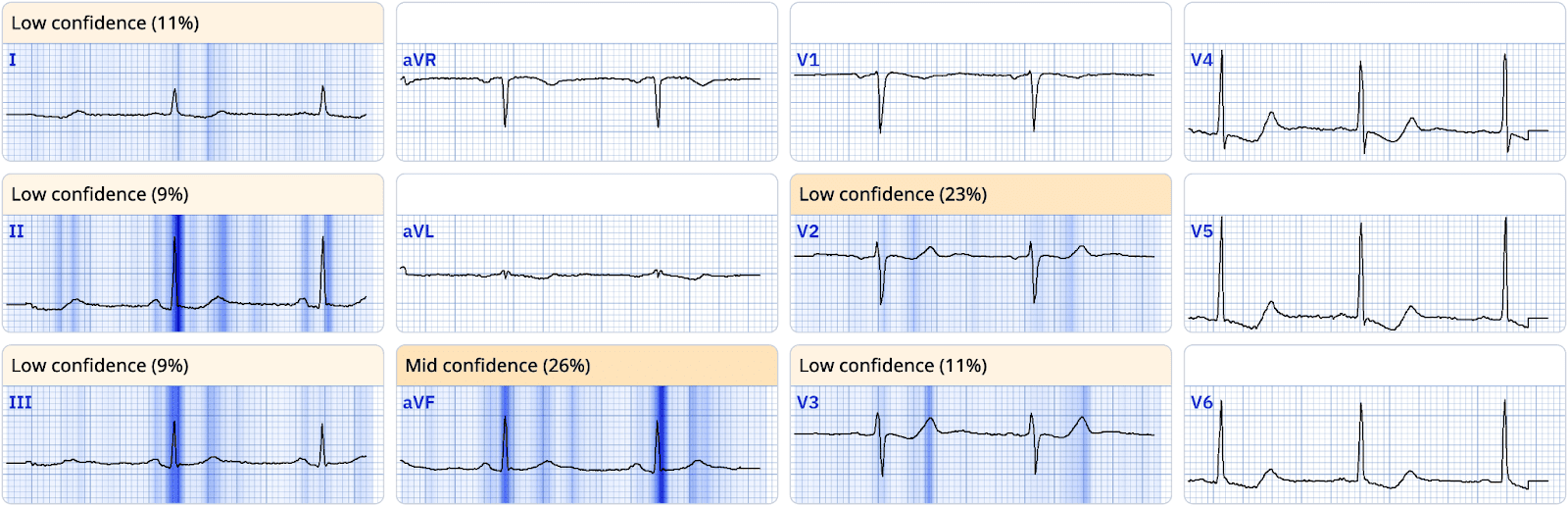
Fifteen minutes after total resolution of pain, ECG3 shows reperfusion T wave inversions in the inferior leads, as well as enlarged T waves in V2-V4 consistent with posterior reperfusion T waves (reciprocal to posterior T wave inversion).
Below is the module output at this time:
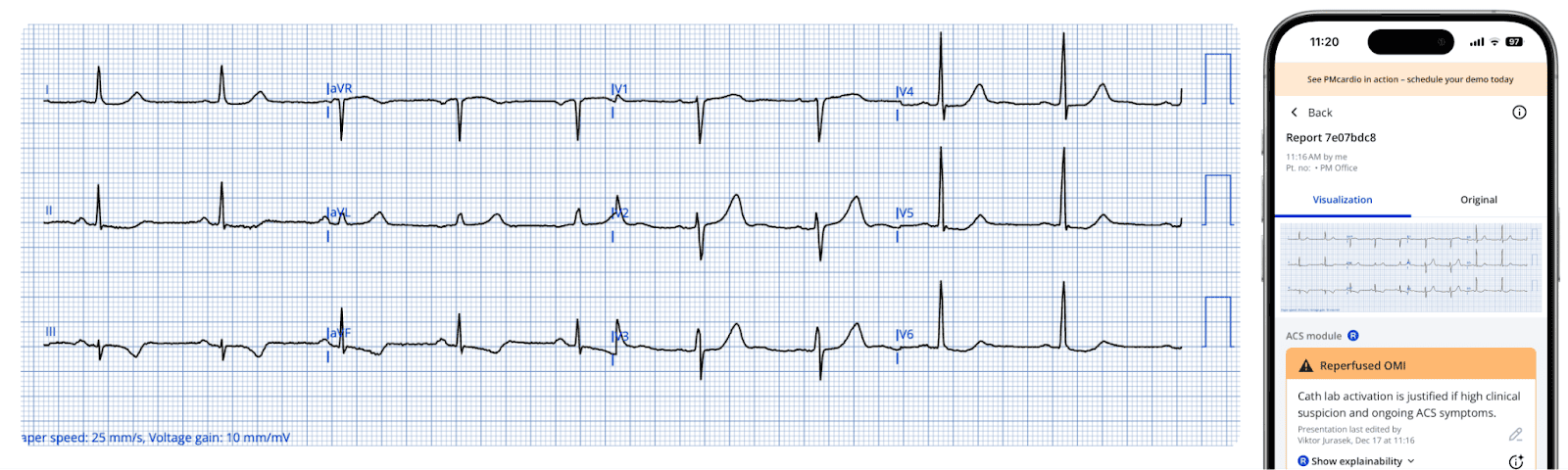
Figure Note: A digitized ECG displaying a diagnosis of Reperfused OMI, as identified by the module.
The module correctly identifies the ECG findings as signs of reperfusion, aligning with the patient’s resolution of symptoms.
The patient was taken urgently to the cardiac catheterization lab, where a culprit lesion in the right coronary artery was identified (noted to be open at the time of the angiogram) and successfully stented.
Optimize STEMI patient pathway with certified AI
The impact of PMcardio at the Cardiovascular Centre Aalst, Belgium:
- 68% reduction in false positive STEMI alerts
- 100% sensitivity in true positive STEMI patients
- 34% reduction in ECG to balloon time for STEMI patients
- 50% decrease in door-to-ECG time month-over-month
References
- Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol. 2000;36(3):970-1062.
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618-e651. doi:10.1161/CIR.0000000000000617
- Hillinger P, Strebel I, Abächerli R, et al. Prospective validation of current quantitative electrocardiographic criteria for ST-elevation myocardial infarction. Int J Cardiol. 2019;292:1-12. doi:10.1016/j.ijcard.2019.04.041.
- Herman R, Meyers HP, Smith SW, et al. International evaluation of an artificial intelligence–powered electrocardiogram model detecting acute coronary occlusion myocardial infarction. Eur Heart J – Digit Health. 2023;5(2):123-133. doi:10.1093/ehjdh/ztad074.
- Macherey-Meyer S, Meyers P, Smith S, et al. Artificial intelligence-based detection of occlusion myocardial infarction: first external validation in a German chest-pain unit cohort. 2024. doi:10.1007/s00392-024-02406-5.
- Garvey JL, Zegre-Hemsey J, Gregg RE, et al. Electrocardiographic diagnosis of acute myocardial infarction in the emergency department: a practical algorithm. J Am Heart Assoc. 2019;8(11):e011629. doi:10.1161/JAHA.118.011629.
- Byrne RA, Ibanez B, James S, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(30):2568-2698. doi:10.1093/eurheartj/ehad191.
- Pires de Morais G, Lopes A, Machado C, et al. Wellens’ syndrome: a pattern to remember. BMJ Case Rep. 2018;2018:bcr-2018-224582. doi:10.1136/bcr-2018-224582.
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary. J Am Coll Cardiol. 2013;61(4):485-510. doi:10.1016/j.jacc.2012.11.018.
- Jollis JG, Roettig ML, Aluko AO, et al. Implementation of a statewide system for STEMI care in North Carolina: program evaluation. JAMA. 2007;298(21):2371-2380. doi:10.1001/jama.298.21.joc70189.