In the realm of cardiology, accurately diagnosing occlusion myocardial infarction (OMI) in patients exhibiting left bundle branch block (LBBB) or ventricular paced rhythms, presents a significant challenge. The Sgarbossa criteria, developed in the 1990s by Dr. Elena Sgarbossa, have significantly contributed to addressing this issue, marking a pivotal advancement in the field1.
The subsequent refinement of these criteria by Dr. Stephen Smith has further improved diagnostic precision, thus improving the accuracy of MI detection2.
This article delves into the essence of the Sgarbossa criteria, their modifications, and their critical role in modern cardiology.
Table of Contents
What is Sgarbossa criteria?
The Sgarbossa criteria as a STEMI Equivalent represent a fascinating facet of ECG patterns, identifying acute coronary occlusion patterns on ECG that don’t fit the typical STEMI mold but demand equally rapid response. These patterns extend beyond conventional criteria, capturing scenarios where the risk and necessary treatment urgency mirror those of STEMI. For a deeper dive into the world of STEMI equivalents :
STEMI Equivalents: Navigating Hidden Indicators of Acute Coronary Occlusion
Among these critical patterns, the Sgarbossa criteria stand out as one of the key tools in recognizing these life-threatening conditions for patients with wide QRS complex morphology3.
How to Identify Sgarbossa Criteria on ECG
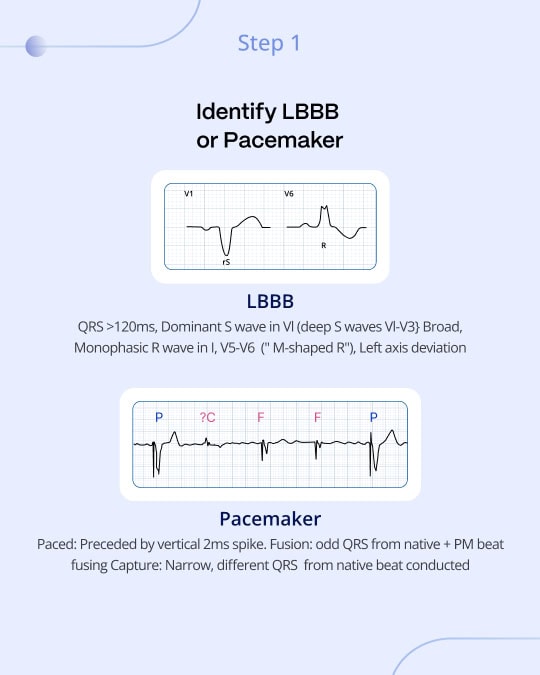
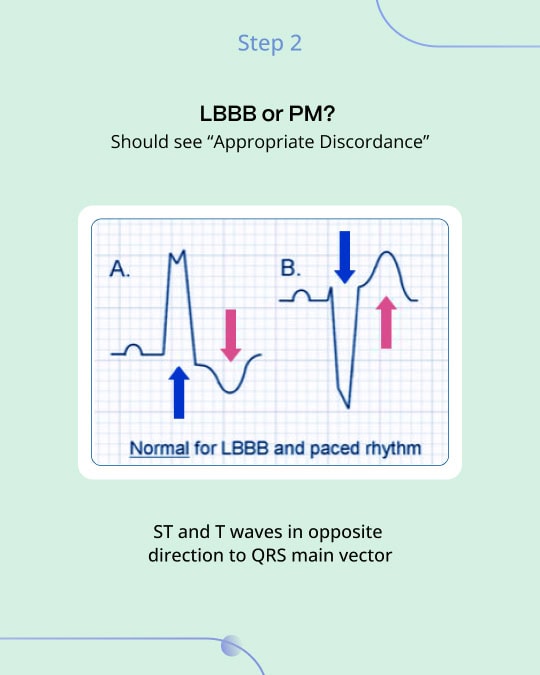
The original Sgarbossa criteria utilized a scoring system from specific ECG findings to diagnose MI in patients with left bundle branch block (LBBB) or those with ventricular paced rhythms1. This method is outlined through three essential components:
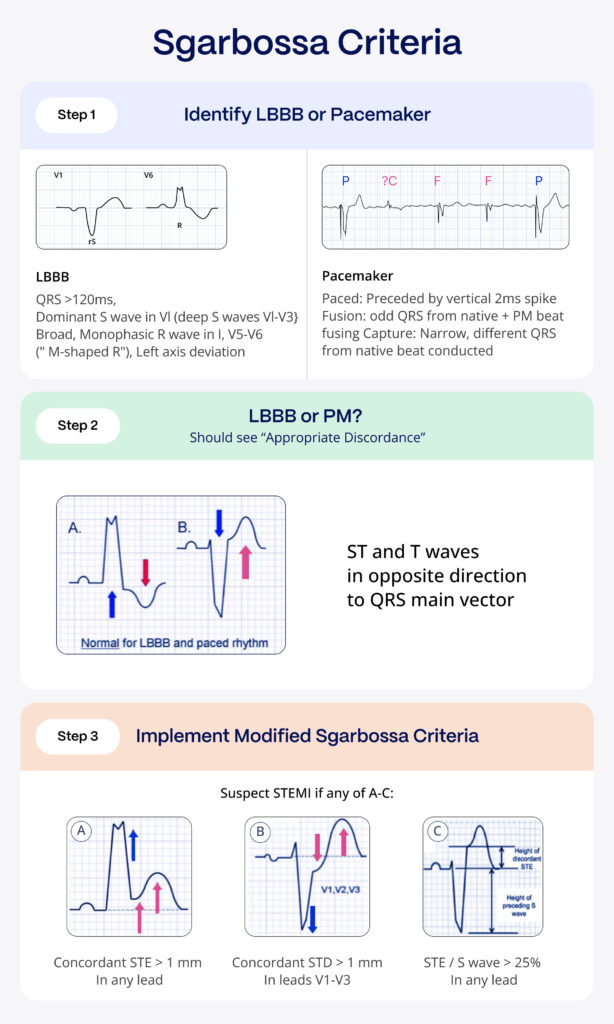
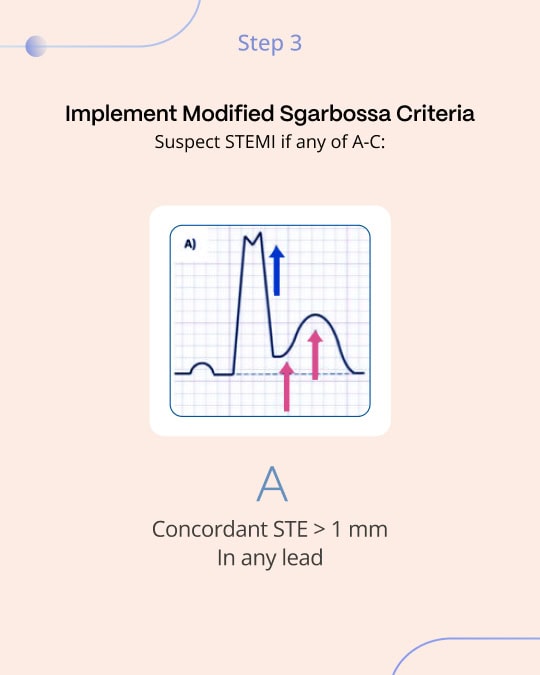
- Concordant ST elevation (ST-segment elevation in the same direction as the major component of the QRS) of 1 mm or more in any lead scores 5 points, highlighting a probable MI.
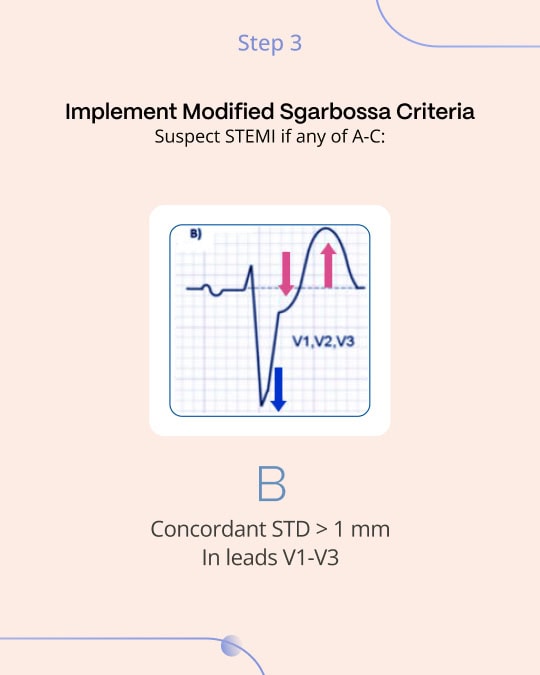
- Concordant ST depression of 1 mm or more in the anterior chest leads (V1-V3) earns 3 points, indicative of posterior OMI. This is directly analogous to the most important features of posterior OMI in narrow complex QRS ECGs: ischemic ST depression maximal in V1-V44.
- Excessively Discordant ST Elevation exceeding 5 mm in leads with a negative QRS complex results in 2 points.
A cumulative score of 3 or more was considered positive by the original Sgarbossa study, providing a high specificity and modest sensitivity for OMI. 3
Sgarbossa Criteria: Step by Step Guide
The Smith-Modified Sgarbossa Criteria: A Leap Forward
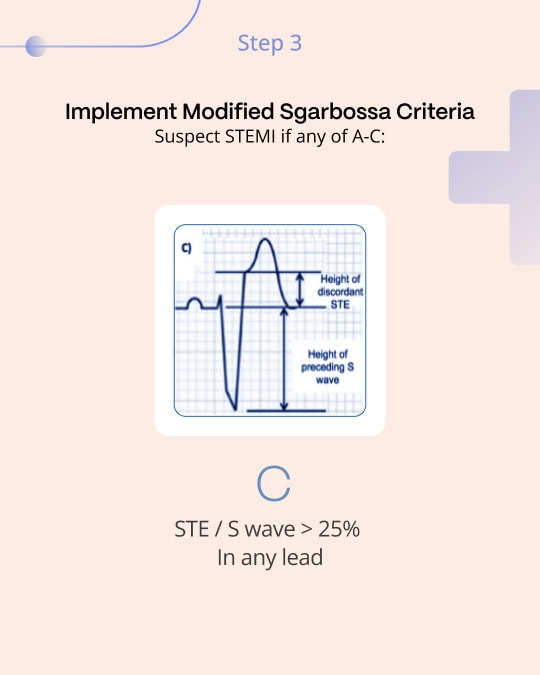
Recognizing the original criteria’s limitations, especially regarding its third rule, the Smith-modified Sgarbossa criteria were introduced. This adaptation replaces the absolute 5 mm excessive discordant ST elevation criterion with a proportional rule: ST segment to S-wave ratio of ≥0.25 in leads with discordant QRS complexes, significantly refining the sensitivity and specificity for MI diagnosis2. This was a key improvement because all ECG findings are proportional, explaining many false positives and false negatives of the original absolute 5 mm criterion.
For example, a patient with a baseline 55 mm S wave in lead V3 would be likely to have more than 5 mm of STE at baseline. On the other hand, a patient with acute LAD occlusion will be unlikely to mount 5 mm of STE in V3 if they only have a 10 mm S wave before the event. Evaluating the STE in relation to its preceding S wave largely solves the problem in both directions.
The Smith-modified Sgarbossa criteria represent a vital advancement in the precise evaluation of ECGs for patients with LBBB or ventricular paced rhythms, equipping healthcare professionals with a more accurate diagnostic tool, enhancing the capability to effectively identify MI.
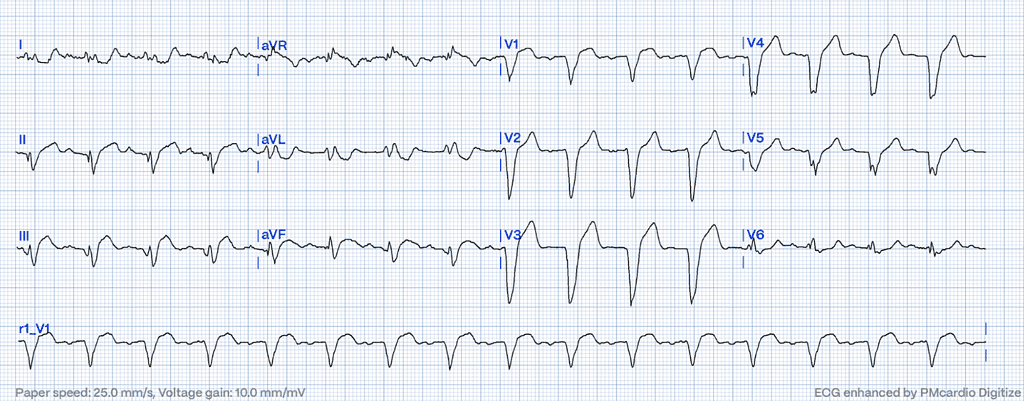
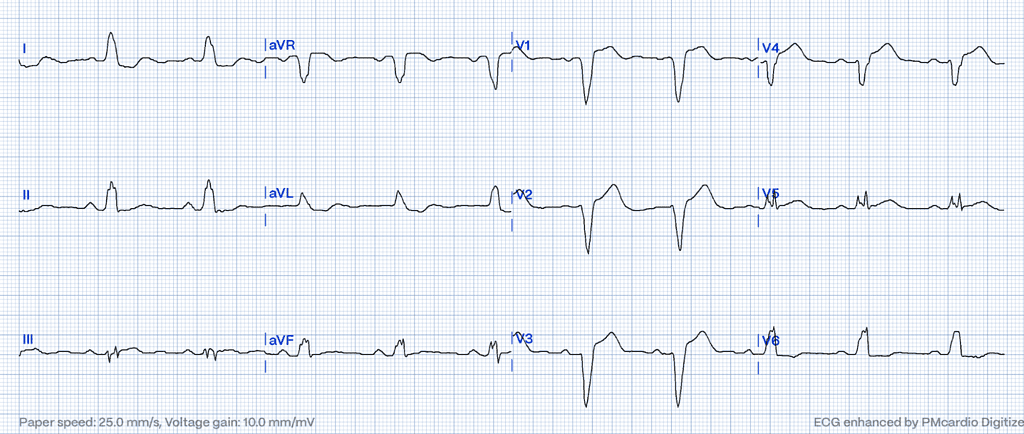
Following figure 1, The modified criteria adeptly identify the subtle yet significant markers of MI that the original criteria might overlook, such as the excessively discordant ST elevation observed in this ECG in leads II, III, and aVF with reciprocal findings in I and aVL. Without the nuanced approach of the Smith-Modified Sgarbossa criteria, this case might have been misclassified as negative for OMI under the original Sgarbossa guidelines due to the lack of concordant ST elevation or depression meeting the 5mm threshold.
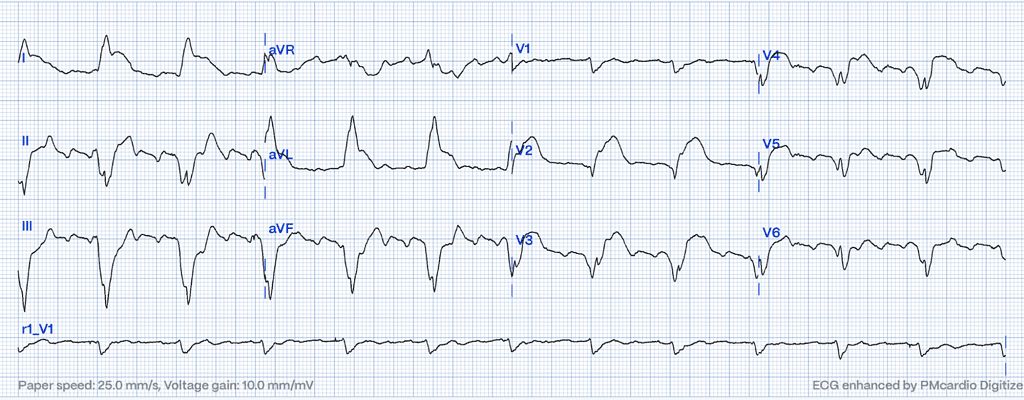
Following figure 2, a possible concordant STE under 1mm appears in V5 and III. In III, STE slightly under 1 mm with an isoelectric QRS suggests OMI, as the ST segment should mirror the QRS’s neutrality. Lead aVL displays at least 1 mm of reciprocal STD with a QRS under 4 mm, marking nearly 30% discordant STD – a strong indicator of OMI.
Challenges in Sgarbossa Criteria Application: The Role of Advanced Technologies and Continuous Education
The application of the Sgarbossa criteria, while invaluable, encounters significant challenges in clinical practice.
One notable limitation is the potential for inter-observer variability, where the subjective nature of ECG interpretation can lead to differences in applying the criteria among healthcare professionals5. This variability underscores the need for extensive training and experience to ensure accurate and consistent use.
STEMI Equivalents: Play It Safe with Certified AI
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- Medical Device Class II(b) EU MDR CE-mark
- 5 FREE ECGs/month - no credit card needed
Additionally, the criteria face difficulties with boundary cases – situations where ECG patterns marginally meet or fall short of the criteria’s thresholds6. These borderline instances necessitate a nuanced approach, often requiring clinicians to integrate additional diagnostic information and rely on their clinical judgment.
The complexity of these challenges highlights the critical need for ongoing research and education to refine diagnostic approaches and enhance the reliability and effectiveness of the Sgarbossa criteria in practice.
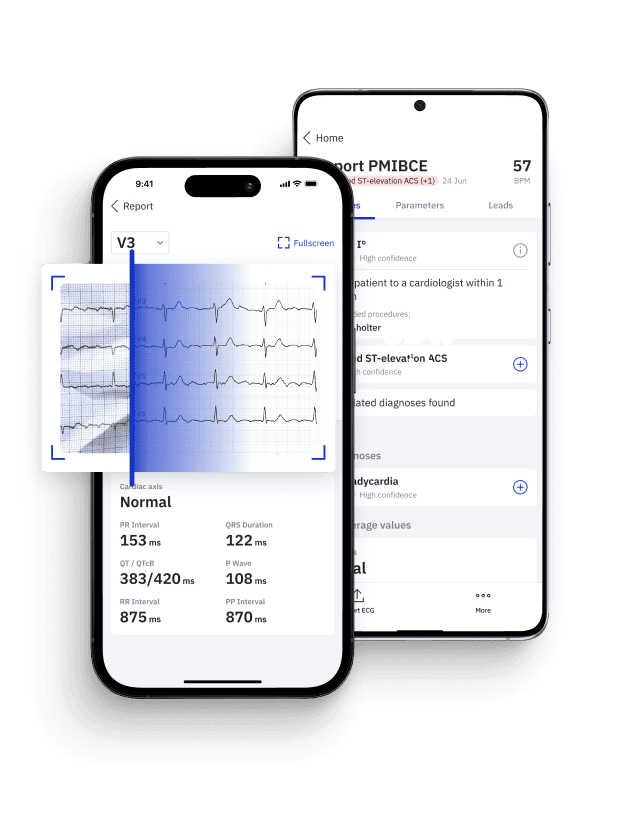
These issues underscore the importance of precision and consistency in ECG interpretation. PMcardio’s advanced deep learning algorithms are designed to mitigate these challenges by offering a validated, reliable, and accurate analysis of ECG patterns8.
From Sgarbossa to AI: Navigating the Future of Cardiac Diagnostics
The journey of cardiac diagnostics from the Sgarbossa criteria to AI-driven models such as PMcardio highlights a transformative era in healthcare. These advancements underscore the shift towards precision medicine, where diagnostic and treatment strategies are increasingly tailored to the individual patient’s specific conditions and needs7.
The development and refinement of the Sgarbossa criteria, the acknowledgment of STEMI equivalents, and the advent of AI technologies like PMcardio collectively enhance our ability to accurately diagnose and treat cardiac events. These tools and methodologies are vital in ensuring timely intervention for MIs, ultimately saving lives and improving patient outcomes.
PMcardio is at the forefront of integrating AI in cardiac diagnostics, exemplifying how technology can augment human expertise.
This article was edited by Dr. H. Pendell Meyers.
Stay on the pulse with our newsletter
- Emerging ECG patterns
- Expert-led webinars
- STEMI management updates
- AI advancements in emergency hospital care
Your submission was successful
References
- Sgarbossa EB, Pinski SL, Barbagelata A, Gates KB, Wagner GS. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med. 1996 Feb 22;334(8):481-7.
- Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block With the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Ann Emerg Med. 2012 Dec;60(6):766-76.
- Meyers HP, Limkakeng AT, Jaffa EJ, Patel A, Theiling BJ, Rezaie SR, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: a retrospective case-control study. Am Heart J. 2015 Dec;170(6):1255-64.
- Meyers HP, Bracey A, Lee D, Lichtenheld A, Li WJ, Singer DD, Rollins Z, Kane JA, Dodd KW, Meyers KE, Shroff GR, Singer AJ, Smith SW. Ischemic ST-segment depression maximal in V1–V4 (versus V5–V6) of any amplitude is specific for occlusion myocardial infarction (versus nonocclusive ischemia). J Am Heart Assoc.
- Das D, McGrath BM. Sgarbossa criteria for acute myocardial infarction. CMAJ. 2016 Oct 18;188(15):E395. doi: 10.1503/cmaj.150195. Epub 2016 Apr 18. PMID: 27091803; PMCID: PMC5056892.
- Sokolove PE, Sgarbossa EB, Amsterdam EA, Gelber R, Lee TC, Maynard C, Richards JR, Valente R, Wagner GS. Interobserver agreement in the electrocardiographic diagnosis of acute myocardial infarction in patients with left bundle branch block. Ann Emerg Med. 2000 Dec;36(6):566-71. doi: 10.1067/mem.2000.112077. PMID: 11097696.
- Koulaouzidis G, Jadczyk T, Iakovidis DK, Koulaouzidis A, Bisnaire M, Charisopoulou D. Artificial Intelligence in Cardiology-A Narrative Review of Current Status. J Clin Med. 2022 Jul 5;11(13):3910. doi: 10.3390/jcm11133910. PMID: 35807195; PMCID: PMC9267740.
- Powerful Medical. Powerful Medical Website. Available from: https://www.powerfulmedical.com/. Accessed April 3, 2024.