Wellens’ Syndrome is a condition representing a reperfusion state post coronary artery occlusion, marked by distinctive ECG changes. This condition demands urgent recognition and intervention to prevent the progression to an extensive anterior wall myocardial infarction (MI)3. This article offers an in-depth look designed for healthcare professionals seeking to understand Wellens’ Syndrome, from its pathophysiology to its management and implications for patient care.
Table of Contents
What is Wellens’ Syndrome: The Basics
The syndrome was first described in the 1980s by Hein J.J. Wellens, a Dutch cardiologist whose work profoundly impacted the understanding and treatment of cardiac ischemia2.
While Wellens’ syndrome is classically associated with the anterior leads, reflecting the area most commonly supplied by the LAD, it’s crucial to acknowledge that ischemic changes can also, albeit less commonly, manifest in other regions of the heart, potentially appearing in inferior or lateral leads under certain conditions.
This variability underscores the importance of a comprehensive clinical and ECG evaluation to identify individuals at risk accurately, highlighting Wellens’ syndrome’s complexity beyond typical anterior lead manifestations1. Wellens’ syndrome, being a reperfusion phenomenon, alerts clinicians to the potential risk of a new occlusion in the critical coronary artery, requiring careful monitoring and immediate intervention to prevent adverse outcomes.
STEMI Equivalents: Miss One and Risk It All!
- Medical Device Class II(b) EU MDR CE-mark
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- 5 free ECG reports - no credit card needed
Key Symptoms and Early Detection
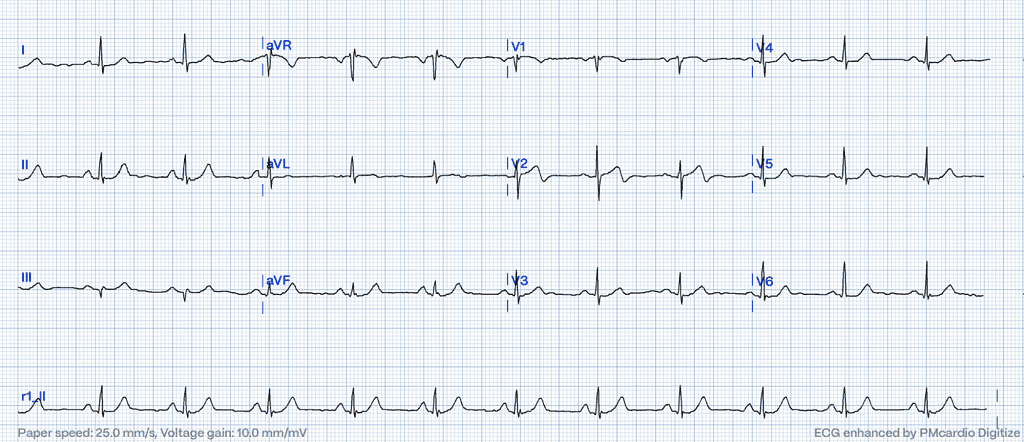
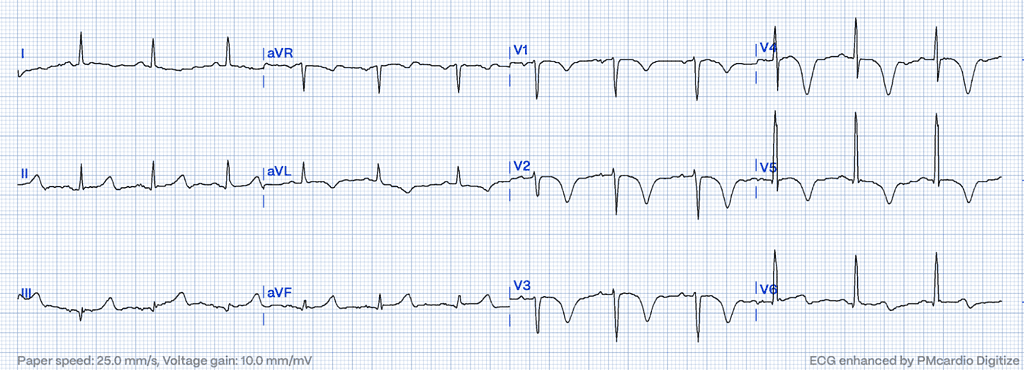
The critical period for recognizing Wellens’ Syndrome on the ECG is often during a pain-free or pain-receding interval, making the respective ECG changes the primary diagnostic clue2. These changes are typically observed in the precordial leads V2-V3 but can extend to V1-V6, manifesting as biphasic or deeply inverted T waves2.
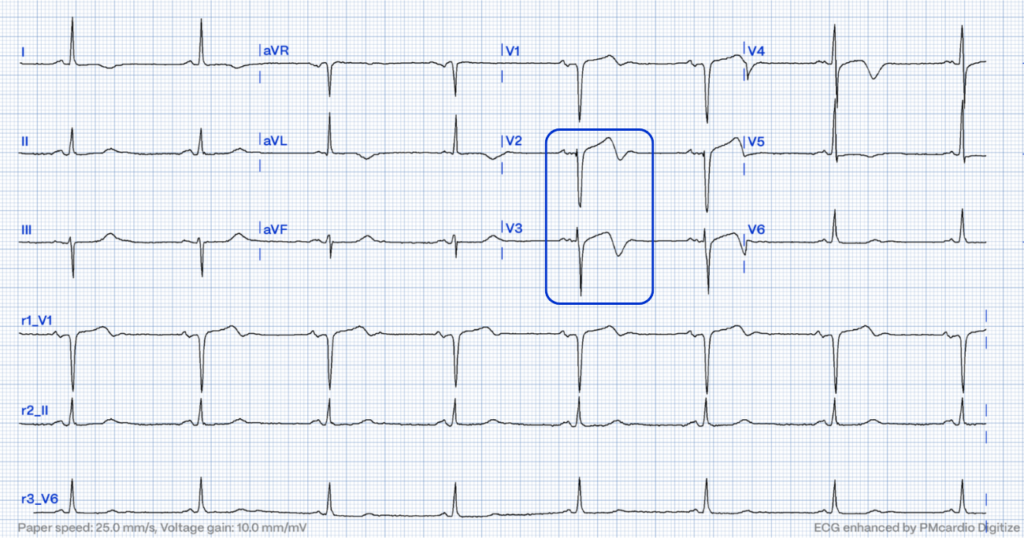
Wellens’ Syndrome ECG: Deciphering the Signs
The hallmark of Wellens’ Syndrome is its ECG pattern, typically divided into two types:
- Type A: Characterized by biphasic T waves in V2-V32 (and possibly extending to V1, V4, V5, and V6)
- Type B: Identified by symmetrically inverted T waves in the same leads2.
It is important to note that the current classification of Wellens’ syndrome into “types” might indeed be somewhat misleading if interpreted strictly as distinct entities. Instead, these classifications could more accurately be described as different stages of the same underlying event – reperfused coronary artery post acute coronary occlusion, reflecting the evolution of myocardial ischemia due to critical stenosis of the LAD artery, rather than fundamentally different conditions. Describing them as stages rather than types underscores the dynamic nature of the syndrome and its progression, highlighting the temporal aspect of ischemic changes over time.
Understanding the Evolutionary Nature of Wellens’ Syndrome
Referring to these presentations as stages rather than types emphasizes the continuum of ischemic injury and potential recovery within the myocardium, which aligns with the pathophysiological understanding of CAD and myocardial ischemia. This perspective also aids in clarifying that Wellens’ syndrome is not a static snapshot but a window into an evolving process.
Enhancing Clinical Approach through Stage-Based Interpretation
Characterizing the different ECG patterns of Wellens’ syndrome as stages rather than types might reduce confusion among clinicians, encouraging a more unified approach to diagnosis and management. It reinforces the necessity of immediate intervention regardless of the “type” observed, as both represent different points along the same pathophysiological continuum. This approach may facilitate a more nuanced understanding of the syndrome, fostering prompt recognition and treatment to prevent the progression of coronary artery disease in affected patients.
It is crucial to note that while this reinterpretation offers a conceptual clarification, the practical clinical approach to identifying and managing Wellens’ syndrome remains critically dependent on recognizing these specific ECG patterns. Regardless of whether they are termed “types” or “stages,” the imperative is the early identification and intervention to mitigate the risk of a subsequent, potentially catastrophic MI.
The Wellens’ Criteria: A Diagnostic Guideline
Clinicians should be vigilant for the Wellens’ warning signs, particularly in patients with a history of chest pain that has resolved by the time of evaluation2. The diagnosis hinges on a constellation of criteria beyond the ECG patterns, which encompass:
- No or minimal elevation in cardiac enzymes3
- No pathological Q waves and an isoelectric or minimally elevated ST segment3
- No loss of precordial R wave progression3
- A history of angina3
- Biphasic or deeply inverted T waves in leads V2-V32,3
Is Wellens Syndrome a STEMI Equivalent?
Despite widespread belief, Wellens’ Syndrome does not classify as one of the STEMI equivalents. It represents a reperfusion phenomenon rather than a sustained, complete coronary occlusion. In Wellens’ syndrome, specific ECG patterns, notably biphasic or deeply inverted T waves in the precordial leads, alert clinicians to severe but reversible ischemic injury due to partial reperfusion of the LAD artery.
STEMI Equivalents: Navigating Hidden Indicators of Acute Coronary Occlusion
While the urgency of management may parallel that of STEMI, the underlying mechanisms and therapeutic targets differ, emphasizing early diagnosis and proactive treatment to prevent progression rather than responding to an established infarction.
Causes and Risk Factors of Wellens’ Syndrome
While the precise cause of the arterial blockage can vary, the progression of atherosclerosis and the likelihood of thrombosis is significantly heightened by several risk factors, including hypertension, hyperlipidemia, smoking, diabetes mellitus, and a sedentary lifestyle, which can contribute to the development of cardiovascular risk factors.
Stay on the pulse with our newsletter
- Emerging ECG patterns
- Expert-led webinars
- STEMI management updates
- AI advancements in emergency hospital care
Your submission was successful
Treatment Pathways and Management Strategies
Some Wellens’ Syndrome patients are potentially at risk of progressing to complete LAD occlusion without proper management, highlighting the importance of vigilant cardiac monitoring and timely intervention. Percutaneous coronary intervention (PCI) is often the treatment of choice, aiming to prevent a significant MI by restoring blood flow through the LAD.
The decision for PCI hinges on a thorough clinical evaluation, including ECG and symptom assessment. Continuous hospital monitoring is essential to detect any deterioration and intervene promptly, thereby averting reocclusion and minimizing myocardial damage5.
The Importance of Early Intervention
Early action significantly improves long-term patient outcomes by reducing complications such as arrhythmias, heart failure, and sudden cardiac death5. Moreover, the quick identification of Wellens’ Syndrome allows for an effective stratification of treatment strategies, ensuring that urgent care resources like coronary angiography and PCI are timely and appropriately allocated5.
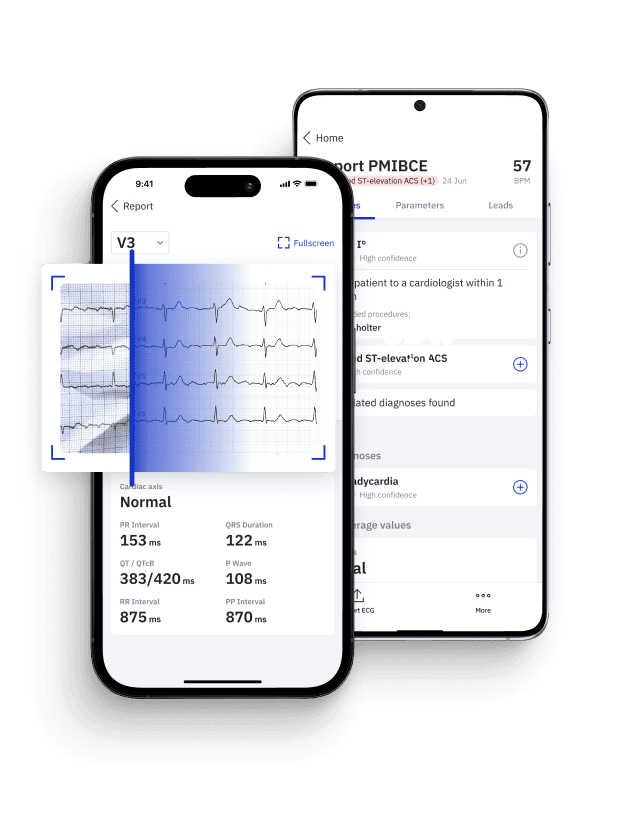
Innovations in Cardiac Care
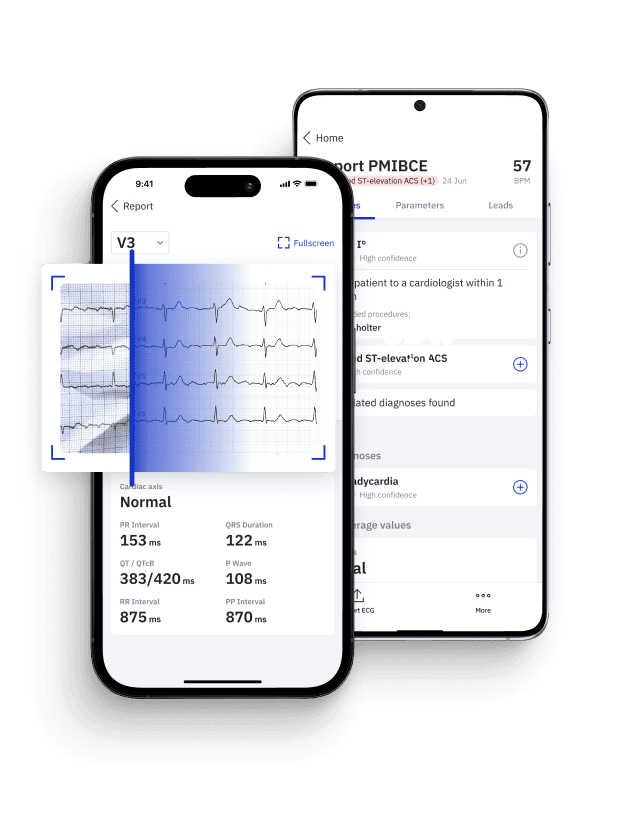
The integration of innovative approaches such as precision medicine, exemplified by AI ECG Interpretation initiatives like PMcardio, offers a new horizon in personalized patient care6. These approaches allow for more nuanced and individualized treatment plans, leveraging the latest in medical research and technology to address the unique aspects of each patient’s condition6. Similarly, the adoption of Occlusion Myocardial Infarction (OMI) protocols underscores the evolution of cardiac diagnostics, moving towards more precise and timely interventions that can drastically improve the management of cardiac events6.
Emphasizing Proactive Cardiac Care
In navigating the complexities of conditions like Wellens’ Syndrome, the move towards these sophisticated diagnostic and treatment methodologies marks a significant advancement in our ability to cater to the specific needs of our patients.
As we continue to evolve in our understanding and management of cardiac conditions, the incorporation of such cutting-edge strategies into everyday practice is not just aspirational but essential. It represents a shift towards a more informed, precise, and patient-centric approach to healthcare that promises better outcomes and a deeper understanding of heart disease’s intricacies and dynamic nature.
STEMI Equivalents: Play It Safe with Certified AI
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- Medical Device Class II(b) EU MDR CE-mark
- 5 free ECG reports - no credit card needed
References
- Tandy TK, Bottomy DP, Lewis JG. Wellens’ Syndrome. Ann Emerg Med. 1999 Mar;33(3):347-51.
- de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982 Apr;103(4 Pt 2):730-6.
- Smith SW, Whitwam WP. Acute Coronary Syndromes. Emerg Med Clin North Am. 2006 May;24(1):53-89, vi.
- Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004;44:E1-E211.
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ. 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec;130(25):e344-426.
- Powerful Medical. Powerful Medical Website. Available from: https://www.powerfulmedical.com/. Accessed March 20, 2024.